Circulation:二尖瓣换瓣术31年后晕厥一例
2013-05-02 Circulation 丁香园
43岁男性,因反复晕厥入CCU治疗。患者9岁时因先天性房室管畸形行肺动脉成形术、机械性二尖瓣置换术,并因完全性房室传导阻滞安装起搏器。入院时患者呈端坐呼吸位,血压78/45mmHg,脉搏72次/分,律不齐。听诊肺部未及干湿罗音,可未及不规则金属瓣膜音。未见四肢水肿。心电图检查提示慢房颤伴间歇期心室起搏心律。INR值高于治疗窗为4.5。心脏超声检查提示二尖瓣间断性开放1:2。Doppler、M-超声
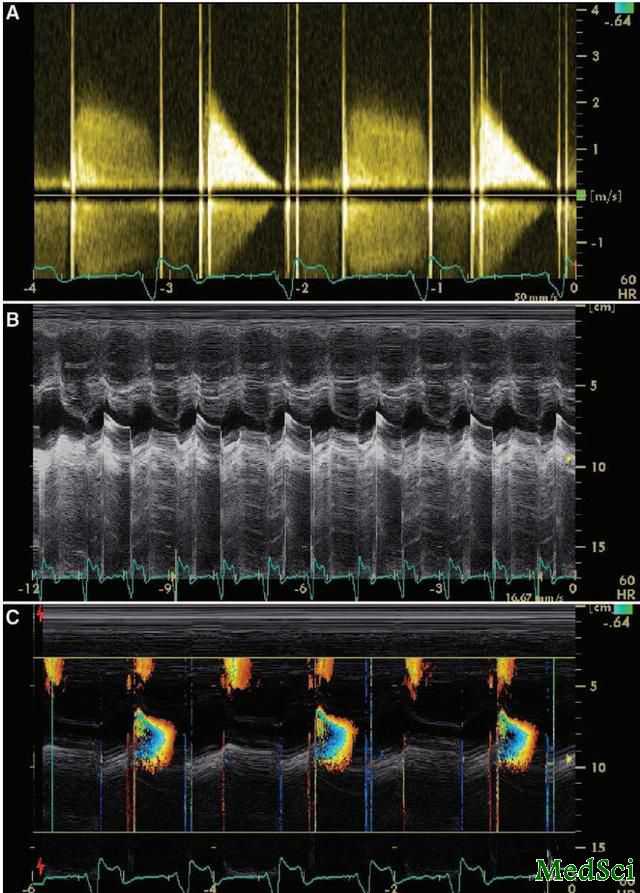
43岁男性,因反复晕厥入CCU治疗。患者9岁时因先天性房室管畸形行肺动脉成形术、机械性二尖瓣置换术,并因完全性房室传导阻滞安装起搏器。入院时患者呈端坐呼吸位,血压78/45mmHg,脉搏72次/分,律不齐。听诊肺部未及干湿罗音,可未及不规则金属瓣膜音。未见四肢水肿。心电图检查提示慢房颤伴间歇期心室起搏心律。INR值高于治疗窗为4.5。心脏超声检查提示二尖瓣间断性开放1:2。Doppler、M-超声、彩色M-超声均证实跨瓣压重度升高20/8mmHg。胸透检查提示二尖瓣假体间歇性开放。
患者接受外科手术治疗时发现,瓣膜表面全部为钙化组织覆盖,阻碍了二尖瓣假体的开放。
二尖瓣假体间断开放较罕见,发生于单叶活动式假体植入后10至23年。本例患者换瓣术后已达31年。一般患者的INR值处于治疗窗内。外科探查发现假体表面翳状物影响瓣膜功能,通常需再次行瓣膜置换术。本例患者瓣膜上的翳状物在手术中完全彻底清除。二尖瓣假体间断开放和容易被漏诊,因其跨瓣压差几乎正常。胸透检查非常有用,但能记录连续心动周期的精确的超声检查也是一项不可替代的技术。
与二尖瓣相关的拓展阅读:

Recurrent Syncope 31 Years After Mitral Valve Replacement
A 43-year—old man was admitted to the coronary care unit because of recurrent syncope. His medical history included pulmonic valve angioplasty at age 9 years, mechanical mitral valve replacement because of severe mitral regurgitation caused by congenital atrioventricular canal, and pacemaker implantation because of complete atrioventricular block. On admission he was orthopneic, his blood pressure was 78/45 mm Hg, and his pulse was 72 beats per minute, irregular. On auscultation, lungs were clear and there were irregular cardiac sounds of mechanical mitral prosthesis. There were no signs of peripheral edema. ECG showed slow atrial fibrillation with intermittent ventricular pacing. International normalized ratio was in high therapeutic range, at 4.5. Echo examination showed intermittent opening of the mitral valve 1:2. This was confirmed by continuous wave Doppler, M-mode echo, and color M-mode echo (Figure) with mildly elevated gradient 20/8 mm Hg. Cine fluoroscopy showed intermittent opening of the mitral prosthesis (online-only Data Supplement Movie I; Bjork -Shiley mono-leaflet tilting disk).
The patient underwent surgery. Massive calcified pannus covered the valve and interfered with the opening of the prosthesis.
Intermittent opening of prosthetic mitral valve is rare1–4 and occurs with mono-leaflet tilting disk prosthesis as in our case, 10 to 23 years after initial surgery; in our case it was 31 years after mitral valve replacement. The international normalized ratio is …
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#换瓣术#
39
#晕厥#
26
#二尖瓣#
29