PNAS阻止癌症转移新武器:纳米材料+激光打断癌细胞的“腿”
2017-06-28 佚名 生物探索
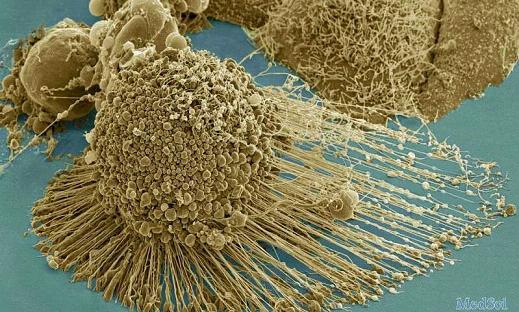
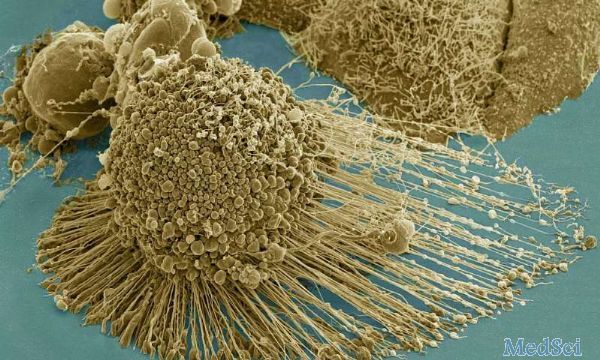
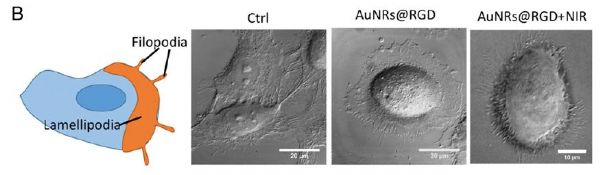
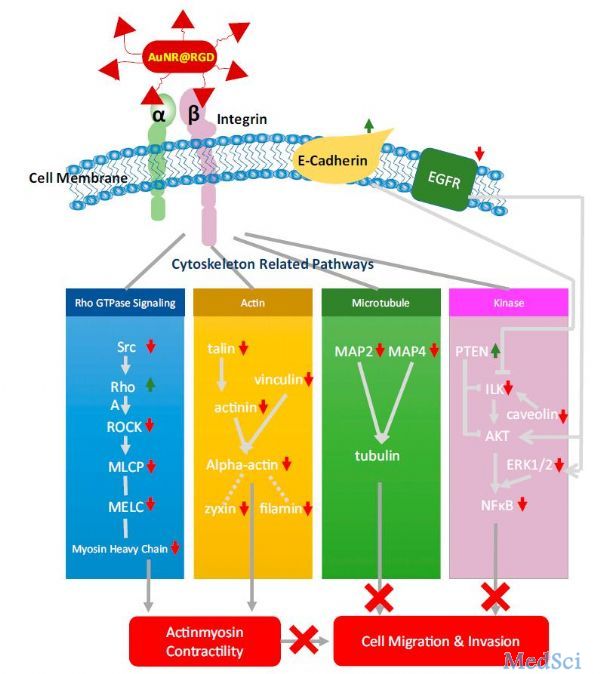
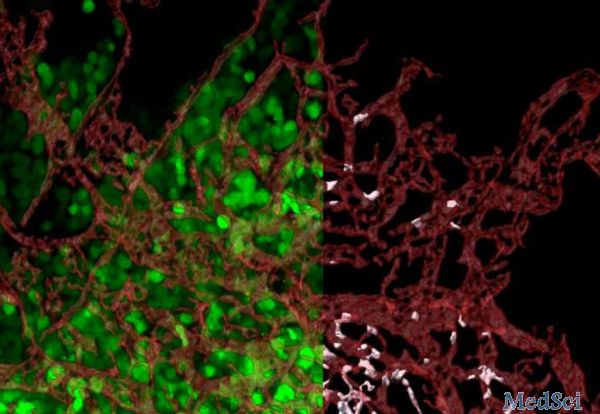
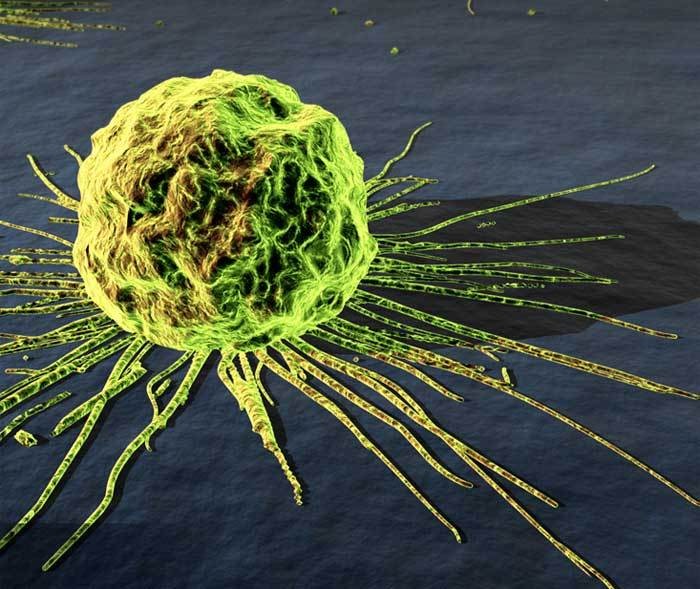
近日,乔治亚理工学院Mostafa El-Sayed教授领导的一个研究小组开发出一种阻止癌症转移的新方法,研究人员利用一种名为光热治疗的方法破坏癌细胞的伪足,阻止细胞迁移,简而言之就是打断癌细胞的“腿”。这项研究于6月27日发表于PNAS上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PNAS#
0
#癌细胞#
24
#激光#
27
#癌症转移#
36
#纳米材料#
40