BJH:重度难治性自身免疫性HIT伴血栓形成的治疗性血浆置换
2021-11-02 MedSci原创 MedSci原创
BJH期刊报告了一例 HITT 病例,案例强调了 TPE 在难治性 HITT 中的快速治疗效果,并强调需要探索 TPE 作为严重 HITT 早期干预的潜在作用
肝素诱导的血小板减少症 (HIT) 是一种高度促血栓形成的疾病,由针对血小板因子 4 (PF4)-肝素复合物的新表位的致病性免疫球蛋白 (Ig) G 引起。在一部分患有血栓形成 (HITT) 的 HIT 患者中,HIT 抗体通过将 PF4 分子与非肝素聚阴离子交联或什至在完全没有聚阴离子的情况下导致血小板活化。虽然停用肝素和开始替代性抗凝治疗仍然是 HITT 的主要治疗方法,但它们不会改变潜在的病理过程,并且可能不适用于难治性 HITT。静脉注射 Ig (IVIg) 和治疗性血浆置换 (TPE) 等辅助疗法可以针对 HIT 的免疫机制进行作用,但在最近的指南中几乎没有指导它们在难治性 HITT 中的应用。
BJH期刊报告了一例 HITT 病例,该病例因暴露于普通肝素 (UFH) 潮红而并发静脉血栓栓塞的进展,尽管使用治疗性磺达肝素和直接凝血酶抑制剂进行治疗。该案例还因 IVIg 和地塞米松的失败以及 TPE 的成功治疗而引人注目。
一名患有 IgG kappa 多发性骨髓瘤且染色体臂 1q 增加的 43 岁女性接受了单采导管放置和非格司亭-sndz(一种非格司亭生物仿制药)的干细胞动员,以收集自体干细胞。她之前接受过硼替佐米、来那度胺和地塞米松的诱导治疗并获得了部分缓解,在收集干细胞时单克隆蛋白从基线 6·74 g/dl 下降到 1·15 g/dl . 2 型糖尿病是她唯一的其他严重合并症。没有静脉血栓栓塞的个人或家族史。
普通肝素冲洗液用于维持单采导管。肝素暴露后 12 天,患者出现单采导管部位疼痛,血小板计数为 12 × 10 9 /l(图 1)。双重超声检查显示右颈内静脉导管相关深静脉血栓形成,计算机断层扫描血管造影显示左下叶肺动脉栓塞。HIT 的 4T 预检分数很高 (7),通过强阳性酶联免疫吸附试验 (ELISA;光密度 3·18) 确认 HIT。血清素释放试验 (SRA) 显示在低剂量肝素(98%,0·1 µ/ml)和高剂量肝素(0%,100 µ/ml)存在的情况下,强烈的血小板活化。
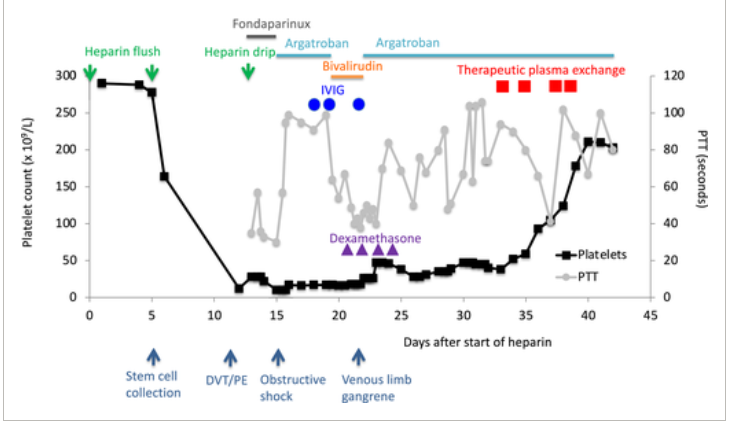
图1:具有连续血小板计数值和部分凝血活酶时间的血栓形成患者的临床过程。PTT,部分凝血活酶时间;DVT,深静脉血栓形成;PE,肺栓塞;IVIG,静脉注射免疫球蛋白
由于没有立即怀疑HIT,患者在入院时首先接受了12小时的治疗性静脉注射uh。然而,抗凝治疗在医院第1天迅速过渡到磺达肝素。经胸超声心动图显示右心室张力,患者因急性肺栓塞恶化而发生梗阻性休克。在发生缺血性肝炎后,抗凝转化为直接凝血酶抑制剂,最初使用阿加曲班(2.5·5 3·5 g/kg/h,持续5天),随后使用比伐卢定(150 250 g/kg/h,持续4天)。患者的血小板计数没有改善,这与难治性 HIT 有关。连续2天ig 1 g/kg/d,血小板计数略有改善,因此,第三次ig 1 g/kg,同时给予地塞米松40 mg /d,连续4天,血小板计数短暂增加至47 109/l。患者肝功能改善,由于难以维持比伐卢定的治疗水平,被转回阿加曲班(2 15 g/kg/h)。同时发现患者肢端缺血性坏死,广泛的深静脉血栓形成,从左腘窝延伸至普通股股,动脉双相正常,符合静脉肢体坏疽的诊断。抗磷脂抗体(抗心磷脂IgM/IgG、-2糖蛋白IgM/IgG)检测阴性。
尽管阿加曲班治疗的部分血小板活酶时间值为 50 - 80 s,但由于持续性血小板减少而导致的严重难治性HIT开始进行血浆置换治疗。患者每隔一天接受4次治疗,血小板计数自第一次TPE后从38升至× 10 9 /l。第4次TPE时,血小板计数由124增至178 × 10 9 /l。继续使用直接凝血酶抑制剂。血浆置换量为1.0体积,由5%白蛋白和50%血浆组成。这种置换液对接受抗凝治疗的凝血病患者有利,因为它可以减少出血和凝血。
在使血小板计数正常化后,鉴于坏疽的存在,患者接受了左跖骨截肢术。在连续 25 天服用阿加曲班后,转为每天服用 20 mg利伐沙班。此后,患者完成了 6 个月的抗凝治疗,没有复发性血栓栓塞或血小板减少症。
案例强调了 TPE 在难治性 HITT 中的快速治疗效果,并强调需要探索 TPE 作为严重 HITT 早期干预的潜在作用。对于难治性 HITT 患者,应考虑 IVIg 和 TPE 以破坏血小板活化,而血小板活化可在肝素停用后继续有效。虽然 TPE 主要在急性或亚急性 HIT 患者的紧急心脏手术前使用,但 TPE 也可能在难治性 HITT 的治疗中发挥重要作用,尽管需要进一步研究以充分阐明这一作用。目前的病例也提醒注意在 HITT 患者中使用磺达肝素。
原始出处:
Bavli, N., Christensen, B., Sarode, R., Hofmann, S. and Ibrahim, I. (2021), Therapeutic plasma exchange in severe refractory autoimmune heparin-induced thrombocytopenia with thrombosis. Br J Haematol. https://doi.org/10.1111/bjh.17917
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
37
#HIT#
0
#治疗性血浆置换#
29
#血浆置换#
36
#难治性#
24
谢谢分享
40