Anesth Analg:甲状腺功能减退并不会导致术后并发症及死亡率的增加
2015-08-28 MedSci MedSci原创
甲状腺功能减退(简称甲减),是由于甲状腺激素合成及分泌减少,或其生理效应不足所致机体代谢降低的一种疾病。临床研究表明,甲状腺功能减退可能与非心脏手术后的死亡率,主要的心血管及感染并发症相关。 东京女子医科大学的研究人员进行了一项回顾性队列研究,研究人员于2005-2012年在克利夫兰诊所,对非心脏手术前6个月内甲状腺浓度可以维持机体代谢的成年人进行了评估。该研究将患者分为3类:(1)甲状
甲状腺功能减退(简称甲减),是由于甲状腺激素合成及分泌减少,或其生理效应不足所致机体代谢降低的一种疾病。临床研究表明,甲状腺功能减退可能与非心脏手术后的死亡率,主要的心血管及感染并发症相关。
东京女子医科大学的研究人员进行了一项回顾性队列研究,研究人员于2005-2012年在克利夫兰诊所,对非心脏手术前6个月内甲状腺浓度可以维持机体代谢的成年人进行了评估。该研究将患者分为3类:(1)甲状腺功能减退组(患者于术前被诊断为甲状腺功能减退,并且术前6个月内TSH 值增加(>5.5mIU/L));(2)治疗组(患者被诊断为甲状腺功能减退,并且TSH值正常[0.4–5.5mIU/L]);(3)甲状腺机能正常组(患者没有被诊断为甲状腺功能减退,并且TSH 值正常)。通过反倾向评分加权对3组患者进行了一对一的比较以观察混杂变量。使用广义估计方程模型对患者院内心血管患病率,手术伤口并发症,感染及死亡率等主要重点进行评估。使用逻辑回归和Cox比例风险回归分析分别对术中血管升压药的使用和住院时间(次要终点)进行评估。
结果显示,3组患者主要终点间不存在显著差异。与治疗组和甲状腺机能正常组患者相比,甲状腺功能减退组患者在手术期间血管升压药的使用量上略有增加。此外,甲状腺功能减退组患者在术后住院的时间要长于治疗组患者。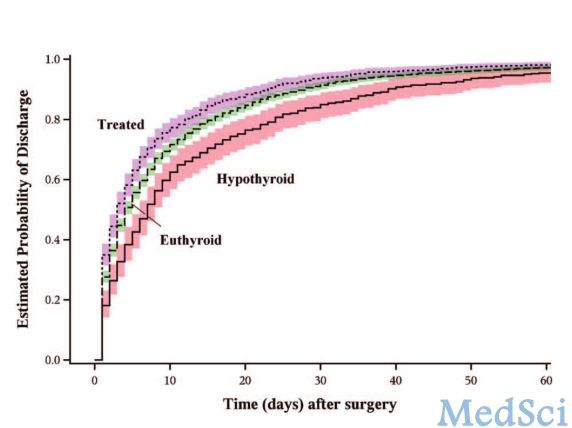
研究人员认为,甲状腺功能减退并不与非心脏手术患者的术后死亡率,伤口及心血管并发症相关。因此,对于将进行非心脏手术的患者来说,推迟手术以进行甲状腺激素替代治疗是没有意义的。
原始出处:
Komatsu R1, You J, Mascha EJ, Sessler DI, Kasuya Y, Turan A.The Effect of Hypothyroidism on a Composite of Mortality, Cardiovascular and Wound Complications After Noncardiac Surgery: A Retrospective Cohort Analysis.Anesth Analg. 2015 Sep;121(3):716-26.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








文章不错,值得拜读
43
赞一个
64
#Anal#
33
#并发#
31
#ANA#
34
#EST#
18