常见消化道瘘的影像学表现--肛瘘
2015-02-03 首都医科大学附属北京朝阳医院 蒋涛 中国医学论坛报
肛瘘主要是由肛周炎症或手术所致,常规瘘管造影和CT检查在肛瘘的诊断和定位以及瘘管的显示方面价值有限,而高场强MRI具有软组织分辨率高、多方位成像的能力,可以清晰显示瘘管、瘘口及肛周炎性反应和肛周脓肿,并可对复杂肛瘘进行分类。我国学者研究表明,磁共振对瘘管的检出率均为100%,对内口的检出率高达95.7%,对脓腔的诊断准确率达100%。 肛瘘的MRI表现取决于肛瘘的分型或分级。依据肛瘘部位
肛瘘主要是由肛周炎症或手术所致,常规瘘管造影和CT检查在肛瘘的诊断和定位以及瘘管的显示方面价值有限,而高场强MRI具有软组织分辨率高、多方位成像的能力,可以清晰显示瘘管、瘘口及肛周炎性反应和肛周脓肿,并可对复杂肛瘘进行分类。我国学者研究表明,磁共振对瘘管的检出率均为100%,对内口的检出率高达95.7%,对脓腔的诊断准确率达100%。
肛瘘的MRI表现取决于肛瘘的分型或分级。依据肛瘘部位和走行,磁共振将其分为5级:1级,单纯线形括约肌间瘘;2级,括约肌内瘘伴脓肿或继发瘘管;3级,非复杂性经括约肌瘘;4级,经括约肌肛瘘伴坐骨直肠脓肿或继发性坐骨直肠瘘管;5级,经肛提肌或肛提肌上瘘伴有或不伴有继发性脓肿。
瘘管在MR表现为T1WI平扫低信号;T2WI显示瘘管较好,呈较高信号,脂肪抑制技术通过抑制肛管和直肠周围脂肪组织使得瘘管显示更加清晰明确,增强扫描T1WI横断位、冠状位和矢状位从不同的方位显示瘘管呈轨道状或管状明显强化,管道内无强化结构考虑为脓液成分,周围炎性反应或脓肿也可出现片状或环形强化。

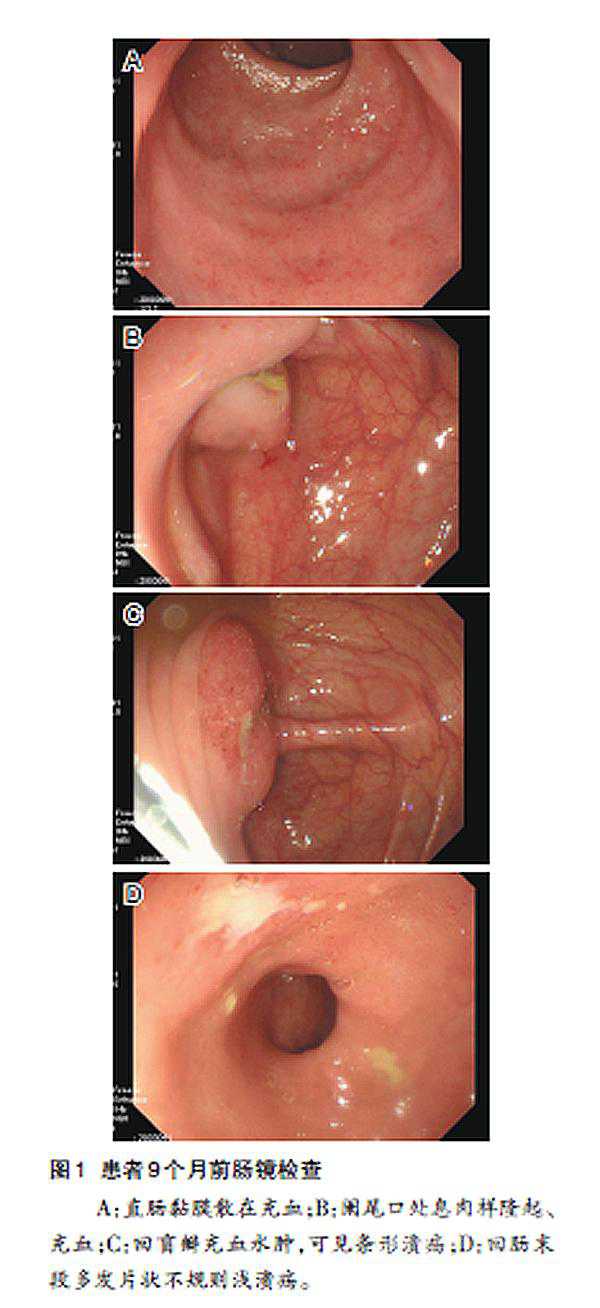
图1 患者男性,46岁。肛瘘,瘘管T2WI呈轨道状低信号,内部可见线状高信号影,增强扫描呈轨道状强化,内部未见明显强化
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









非常好的文章,学习
116
?学习了
124
#肛瘘#
49
#消化道#
38