Lancet Haematol:利妥昔单抗一线治疗滤泡性淋巴瘤:皮下vs静脉
2017-07-17 梁舒瑶 吴星 环球医学
2017年6月,发表在《Lancet Haematol》的一项随机开放标签3期研究调查了皮下利妥昔单抗vs静脉利妥昔单抗一线治疗滤泡性淋巴瘤的有效性和安全性。 背景:静脉利妥昔单抗是B细胞非霍奇金淋巴瘤的标准治疗方法,且给药1.5~6 h。皮下注射制剂可以降低患者的治疗负担,改善卫生保健资源的利用。研究者旨在展示皮下注射利妥昔单抗相对于静脉利妥昔单抗治疗滤泡性淋巴瘤的药代动力学非劣效性,并提供有
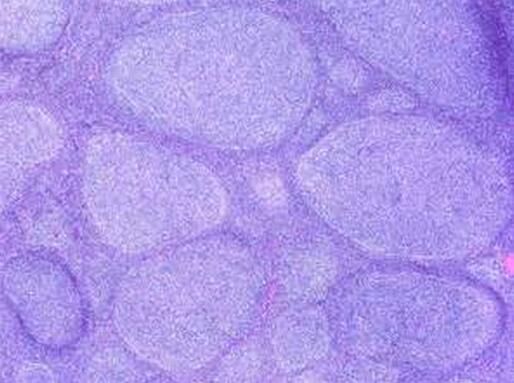
2017年6月,发表在《Lancet Haematol》的一项随机开放标签3期研究调查了皮下利妥昔单抗vs静脉利妥昔单抗一线治疗滤泡性淋巴瘤的有效性和安全性。
背景:静脉利妥昔单抗是B细胞非霍奇金淋巴瘤的标准治疗方法,且给药1.5~6 h。皮下注射制剂可以降低患者的治疗负担,改善卫生保健资源的利用。研究者旨在展示皮下注射利妥昔单抗相对于静脉利妥昔单抗治疗滤泡性淋巴瘤的药代动力学非劣效性,并提供有效性和安全性数据。
方法:在30个国家113个中心,开展一项2阶段、随机、开放标签3期SABRINA研究。年龄在18岁或以上,经过组织学确定,未曾接受过治疗,CD20-阳性1级、2级或3a级滤泡性淋巴瘤;东部肿瘤协作组体能状况为0~2;二维测量的疾病(CT或MRI);预期寿命为6个月或更长;28天或更久时间充足的血液功能;以及根据滤泡性淋巴瘤调查管理指南(Grouped'Etudes des Lymphomes Folliculaires)需要进行治疗的1个或更多症状的患者符合纳入标准。由调查者或研究组成员通过动态随机化算法,将患者随机分配(1:1)至375 mg/m2静脉利妥昔单抗或1400 mg皮下利妥昔单抗,联合化疗(环磷酰胺、阿霉素、长春新碱和泼尼松 [CHOP] 6~8个周期或环磷酰胺、长春新碱和泼尼松 [CVP] 8个周期),诱导期每3周1次,随后每8周维持利妥昔单抗。通过筛选化疗、滤泡性淋巴瘤国际预后指数和地域对随机化进行分层。2阶段的主要终点为诱导末期的总应答(即核定的完全应答、未核定的完全应答和部分应答)。在意向治疗人群中进行有效性分析。报告了基于最后一个完成维持阶段研究的患者临床截止日期的1阶段和2阶段合并数据。该试验在ClinicalTrials.gov注册,编号为NCT01200758,不再招募新患者,但一些患者仍然正在随访中。
结果:2011年2月15日至2013年5月15日期间,随机分配410例患者,205例患者接受静脉利妥昔单抗,205例接受皮下利妥昔单抗。诱导结束时调查者评价的总应答为:静脉组84.9%(95% CI 79.2~89.5),皮下组84.4%(78.7–89.1)。两组的不良事件频率相似(静脉组210例中199 例 [95%] vs 皮下组197 例中189例 [96%]);3级及以上不良事件频率也相似(116 [55%] vs 111 [56%])。最常见的3级及以上不良事件为中性粒细胞减少,静脉组发生44例(21%), 皮下组发生52例(26%)。静脉组有72例(34%)患者发生严重不良事件,皮下组有73例(37%)患者发生严重不良事件。静脉组73例(35%)患者中发生药物相关反应,皮下组95例(48%)患者发生药物相关反应(主要为1级或2级局部注射部位反应)。
阐释:静脉和皮下利妥昔单抗的疗效和安全性相似,未注意到新的安全性隐患。与化疗联合时,皮下给药并不降低抗淋巴瘤的活性。
原始出处:
Davies A, Merli F, et al. Efficacy and safety of subcutaneous rituximab versus intravenous rituximab for first-line treatment of follicular lymphoma (SABRINA): a randomised, open-label, phase 3 trial. Lancet Haematol. 2017 Jun;4(6):e272-e282. doi: 10.1016/S2352-3026(17)30078-9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
27
#HAE#
30
#利妥昔#
18
#静脉#
27
学习了,谢谢
47
#滤泡性淋巴瘤#
32
#EMA#
25