NEJM:Gartners导管囊肿-案例报道
2017-04-06 xing.T MedSci原创
Gartner’s导管囊肿是一种良性阴道囊性结构,是起源与中肾(吴氏)导管残留部位,在男性胚胎发育时,该结构形成精囊、输精管、附睾。Gartner’s导管是位于尿道两侧的成对结构,当囊肿变大时,正如该患者,它们可以出现在中线。患者术后无明显并发症,术后6周无复发迹象。
患者为一名29岁的女性,在不复杂的阴道分娩后4个月发现从阴道内突出一个肿块而到妇科门诊就诊。她没有报告有尿路症状或异常阴道分泌物。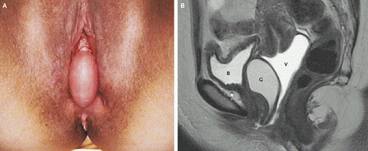
体格检查发现为一平滑、无压痛性肿块,最长直径5厘米,在阴道的前壁中线(如图A所示)。没有证据表明盆腔器官脱垂。膀胱镜检查未发现尿道或膀胱憩室。骨盆(如图B所示)磁共振成像并往阴道打入造影剂显示该病变为一囊性结构(G)位于膀胱(B)和阴道(V)之间。该患者接受囊肿完全切除术,组织学证实是一个Gartner’s导管囊肿。
Gartner’s导管囊肿是一种良性阴道囊性结构,是起源与中肾(吴氏)导管残留部位,在男性胚胎发育时,该结构形成精囊、输精管、附睾。Gartner’s导管是位于尿道两侧的成对结构,当囊肿变大时,正如该患者,它们可以出现在中线。患者术后无明显并发症,术后6周无复发迹象。
原始出处:
Jacob P. Hoogendam,et al. Gartner’s Duct Cyst. N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMicm1609983
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#ERS#
33
#囊肿#
29
#ART#
31