奥拉帕利新适应症上市申请拟纳入优先审评,治疗前列腺癌
2021-01-22 医药魔方 医药魔方
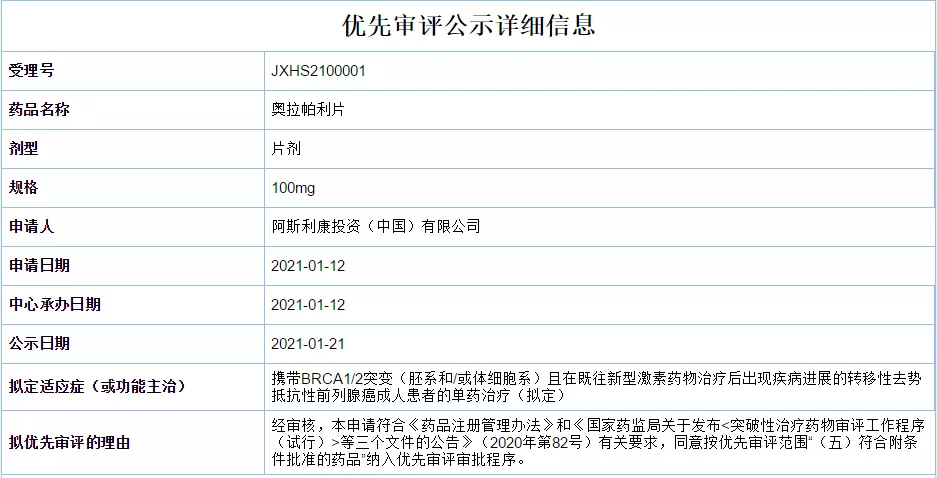
1月21日,CDE官网显示阿斯利康奥拉帕利片新适应症上市申请拟纳入优先审评,单药用于治疗携带BRCA1/2突变(胚系和/或体细胞系)且在既往新型激素药物治疗后出现疾病进展的转移性去势抵抗性前列腺癌成人
1月21日,CDE官网显示阿斯利康奥拉帕利片新适应症上市申请拟纳入优先审评,单药用于治疗携带BRCA1/2突变(胚系和/或体细胞系)且在既往新型激素药物治疗后出现疾病进展的转移性去势抵抗性前列腺癌成人患者。
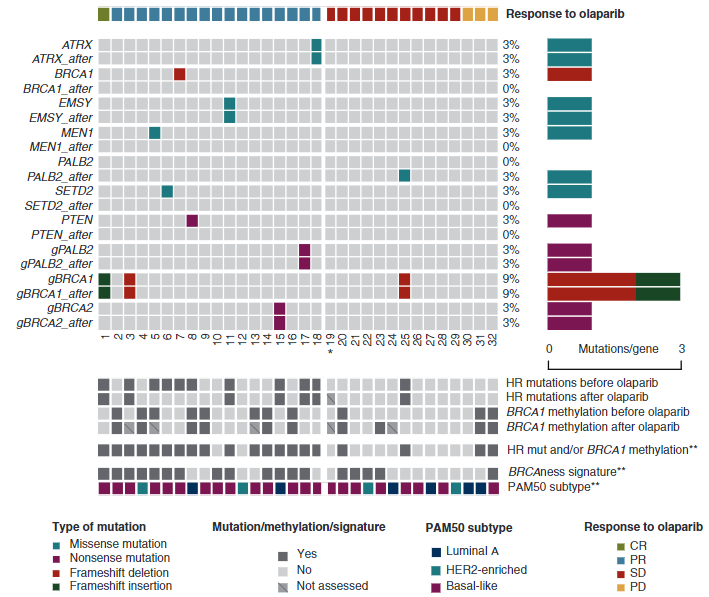
奥拉帕利是FDA批准的首个口服多腺苷二磷酸核糖聚合酶(PARP)抑制剂,通过抑制PARP酶活性和防止PARP与DNA解离,协同DNA损伤修复功能缺陷,杀死肿瘤细胞。最早于2014年先后在欧盟和美国获批上市。
医药魔方NextPharma数据库显示,2019年奥拉帕利分别为阿斯利康和默沙东带来了11.98亿美元和4.44亿美元营收。
奥拉帕利于2018年8月首次获NMPA批准上市,截止目前已在国内获批用于治疗:①铂敏感的复发性上皮性卵巢癌、输卵管癌或原发性腹膜癌成人患者在含铂化疗达到完全缓解或部分缓解后的维持治疗。②BRCA突变晚期卵巢癌的一线维持治疗。③携带BRCA突变的晚期上皮性卵巢癌、输卵管癌或原发性腹膜癌的维持治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#优先审评#
38
#适应症#
33
#新适应症#
33
前列腺癌相关研究,学习了,谢谢梅斯
50
#奥拉帕利#
131