血管特异性炎症标志物:脂蛋白相关磷脂酶A2
2021-12-13 南方七院订阅号 南方七院订阅号
Lp-PLA2有助于远期风险评估,如与hs-CRP联合检测可提高预测价值。
脂蛋白相关磷脂酶
A2(Lp-PLA2)
检验项目有没有一个“福尔摩斯式”的可靠指标,能预测心脑血管疾病风险,使得医生能够及时干预病情进展呢?
当然有,脂蛋白相关磷脂酶A2是心脑血管健康的‘得力管家’,可以预测心脑血管疾病风险。
心脑血管疾病
近年来,我国心脑血管疾病负担日渐加重,现有患病人数约2.9亿,已成为中国人群健康的“头号杀手”。其中脑卒中1300万,冠状动脉粥样硬化性心脏病1100万,动脉粥样硬化性心血管疾病是主要致死和致残原因。
目前,国内外指南均建议采用传统危险因素为基础的模型预测动脉粥样硬化性心血管疾病风险。但仅采用传统危险因素仍存在不足,例如危险因素相同的个体发生心脑血管疾病风险存在差异、某些无传统危险因素的患者仍发生心脑血管疾病等。
生物标志物被认为是传统危险评估的重要补充,脂蛋白相关磷脂酶A2 是血管特异性炎症标志物,国际权威指南一致推荐其用于评估动脉粥样硬化相关的冠心病、缺血性脑卒中及各种血栓性疾病的风险。

脂蛋白相关磷脂酶A2 (Lp-PLA2)是什么?
Lp-PLA2是磷脂酶超家族中的亚型之一,也被称为血小板活化因子乙酰水解酶,由血管内的巨噬细胞、T细胞和肥大细胞分泌。动脉粥样硬化斑块中Lp-PLA2表达上调,且在易损斑块的巨噬细胞中强表达,也是易损斑块的炎症标志物。Lp-PLA2与ox-LDL有较强的亲和力,水解ox-LDL生成溶血卵磷脂和氧化脂肪酸,因此具有很强的促炎症和促动脉粥样硬化的作用。
Lp-PLA2与心血管疾病存在什么关系呢?
动脉粥样硬化(AS)是心脑血管疾病的病理基础。研究发现,炎性细胞及其释放的产物是最主要的促AS的因素,参与粥样斑块的形成、进展过程。大量研究证实Lp -PLA2参与了AS形成、发展等各个阶段,具有促炎症和促动脉粥样硬化的作用,是AS的特异性炎症标志物。
检测Lp-PLA2有什么意义呢?
1、用于评估动脉粥样硬化的炎症程度及其稳定性,是冠心病和缺血性脑卒中动脉粥样硬化相关疾病的临床超前预测指标。
2、是冠心病和缺血性脑卒中的独立预测指标。
3、可预警心肌梗死和脑血栓的发生,对预防心脑血管突发事件具有重要的意义。
4、可用于判断心脑血管栓塞性疾病的复发风险及评估治疗效果。
检测结果如何看?
Lp-PLA2水平存在性别差异,女性低于男性,正在接受激素替代治疗的女性Lp-PLA2水平较低。国内研究提示Lp-PLA2水平<175 ng/mL 为正常,高于175ng/ml提示动脉可能有粥样硬化炎症,且炎症与Lp-PLA2的含量成正比。
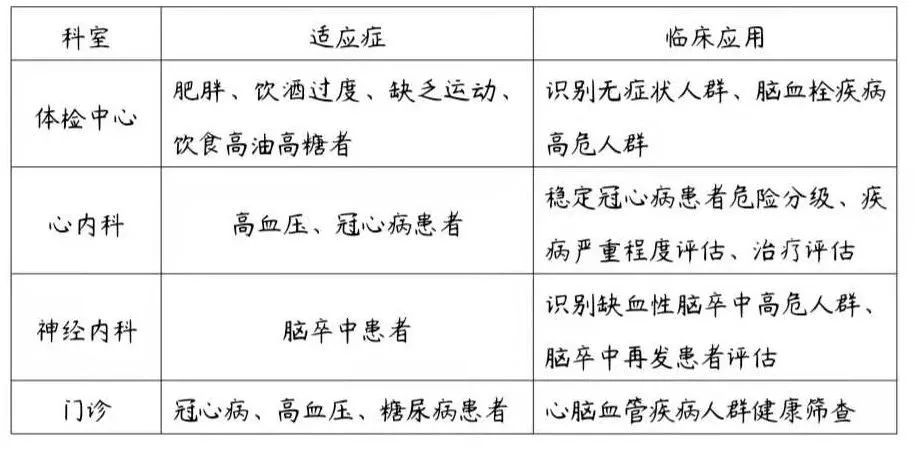
哪些人群需要检测Lp-PLA2呢?
《脂蛋白相关磷脂酶A2临床应用中国专家建议》推荐以下人群可检测Lp-PLA2水平以预测心脑血管疾病风险:
1、无症状高危人群的筛查,尤其是动脉粥样硬化性心血管疾病中危人群。在传统危险因素评估的基础上检测Lp-PLA2以进一步评估心血管疾病风险;
2、已接受他汀类药物治疗且胆固醇水平控制较好的患者。Lp-PLA2水平可提高心血管病事件风险预测价值;
3、发生急性血栓事件的患者,包括急性冠脉综合征(ACS)和动脉粥样硬化性缺血性卒中患者。Lp-PLA2有助于远期风险评估,如与hs-CRP联合检测可提高预测价值。
临床应用科室
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特异性#
44
#炎症标志物#
52
#标志物#
31
#脂蛋白#
46