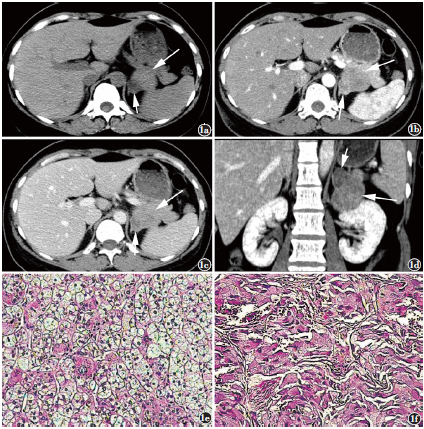
肾上腺碰撞瘤CT表现一例
2018-12-17 覃夏丽 温祖光 黄仲奎 影像诊断与介入放射学,
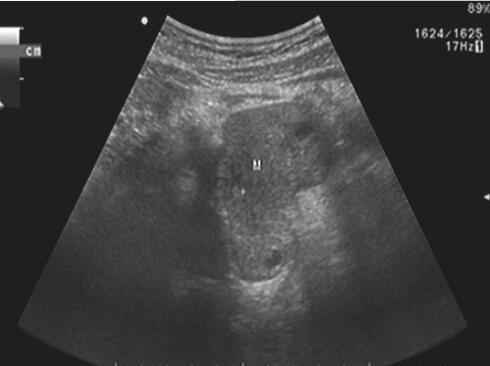
肾上腺碰撞瘤(adrenal collision tumor)较罕见,源于皮质腺瘤和髓质的嗜铬细胞瘤的肾上腺碰撞瘤仅见一例报道。笔者回顾性分析一例肾上腺碰撞瘤的临床及CT表现,旨在增加对肾上腺碰撞瘤的认识。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#碰撞瘤#
36
#肾上腺#
26
照片能不能放大浏览
51
#CT表现#
47
学习了
59