Diabetologia:巨噬细胞中h-铁蛋白的缺失可以减轻小鼠高脂饮食引起的肥胖和糖尿病
2020-11-30 MedSci原创 MedSci原创
铁蛋白是一种储存铁的蛋白质,在铁代谢中起着至关重要的作用。铁积累影响肥胖和糖尿病,这两种疾病都可以通过铁的减少而得到改善。
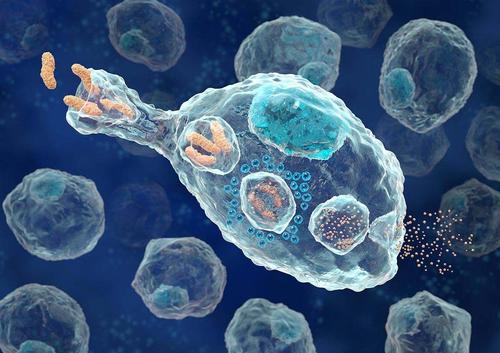
铁蛋白是一种储存铁的蛋白质,在铁代谢中起着至关重要的作用。铁积累影响肥胖和糖尿病,这两种疾病都可以通过铁的减少而得到改善。铁蛋白通过其铁氧化酶活性来降低毒性,从而发挥细胞保护作用。研究人员研究了巨噬细胞h -铁蛋白在肥胖症和糖尿病中的作用。
使用条件巨噬细胞特异性h-铁蛋白(Fth,又称Fth1)敲除(LysM-Cre Fth KO)小鼠,分为正常饮食(ND)野生型(WT)和LysM-Cre Fth KO小鼠,高脂饮食(HFD)野生型(WT)和LysM-Cre Fth KO小鼠。研究人员分析了这些小鼠的肥胖和糖尿病特征、组织铁含量、炎症、氧化应激、胰岛素敏感性和代谢测量。体外实验选用RAW264.7巨噬细胞。
LysM-Cre Fth KO小鼠巨噬细胞铁浓度降低,运铁素mRNA表达升高。HFD-induced肥胖低LysM-Cre Fth KO小鼠比WT老鼠在12周(体重:KO 34.6±5.6 g vs WT 40.1±5.2 g),信使rna表达炎性细胞因子和渗透的脂肪组织巨噬细胞和氧化应激增加HFD-fed WT老鼠,但并不升高HFD-fed LysM-Cre Fth KO小鼠。然而,以HFD喂养的野生型小鼠脂肪组织和脾脏中的铁浓度升高,而以HFD(脂肪组织[白摩铁/g蛋白]]喂养的LysM-Cre Fth KO小鼠并没有观察到这一现象(KO 1496±479 vs WT 2316±866;脾脏[mol Fe/g蛋白]:KO 218±54 vs WT 334±83)。此外,HFD对WT小鼠的糖耐量和胰岛素敏感性均有损害,但在LysM-Cre Fth KO小鼠中有所改善。高温fd下KO小鼠的能量消耗、产热基因的mRNA表达和体温均高于高温fd下WT小鼠。体外实验表明,在转染Fth siRNA的巨噬细胞系中,铁含量降低,脂多糖诱导的Tnf- a (Tnf) mRNA的上调被抑制。
巨噬细胞h -铁蛋白的缺失通过降低细胞内铁水平抑制炎症反应,从而预防手足口病引起的肥胖和糖尿病。这项研究的结果强调巨噬细胞铁水平是肥胖症和糖尿病的潜在治疗靶点。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
32
#BET#
45
#高脂#
33
谢谢MedSci提供最新的资讯
46
学习了
72
学习了,涨知识了!
88