Cell:无间道!包庇癌细胞的它,竟能变成抗癌斗士?
2017-06-19 药明康德 学术经纬
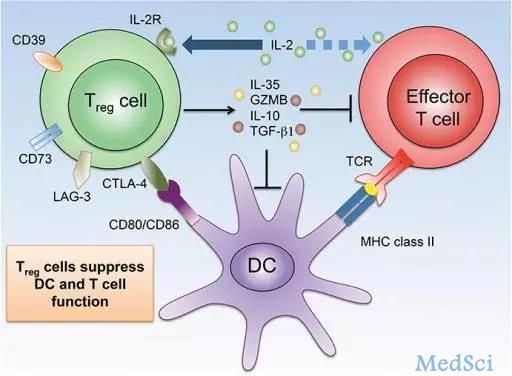
最近,匹兹堡大学(University of Pittsburgh)的研究人员发现了一个可充分释放免疫疗法药物抗癌潜力的线索。这项在《细胞》杂志上发表的工作显示,靶向调节性T细胞(Treg)可能是治疗癌症的有效方法。文章同时还揭示了目前免疫疗法药物的一种重要作用机制,并提供了使其变得更有效的思路。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
28
#Cell#
29
#癌细胞#
29
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
77
很有意思的研究,学习了
71