Blood:SOX11可放大BCR信号,促进MCL样肿瘤细胞进展
2018-04-04 MedSci MedSci原创
中心点:B细胞特异性过表达SOX11可促进B1a B细胞致瘤性增殖,并驱动出现MCL样表型。SOX11过表达与通过BCR信号增强的信号通路相关,BCR信号可被药物BTK抑制剂逆转。摘要:套细胞(MCL)的特点是B细胞受体(BCR)信号增强,应用BTK抑制剂治疗MCL患者可获得积极的治疗效果。但对导致MCL发生BCL信号增强的潜在机制尚不明了,尤其是在其他的淋巴瘤中,BCR信号上游调控子(如CD79
中心点:
B细胞特异性过表达SOX11可促进B1a B细胞致瘤性增殖,并驱动出现MCL样表型。
SOX11过表达与通过BCR信号增强的信号通路相关,BCR信号可被药物BTK抑制剂逆转。
摘要:
套细胞(MCL)的特点是B细胞受体(BCR)信号增强,应用BTK抑制剂治疗MCL患者可获得积极的治疗效果。但对导致MCL发生BCL信号增强的潜在机制尚不明了,尤其是在其他的淋巴瘤中,BCR信号上游调控子(如CD79A)上常可观察到突变,但在MCL中罕见。
在大多数(78-93%)MCL患者中,转录因子SOX11过表达,被认为是MCL特异性致癌基因。迄今为止,由于缺乏合适的动物模型,对SOX11在活体内功能的研究一直停滞不前,因为敲除生殖细胞的SOX11可致胚胎死亡。
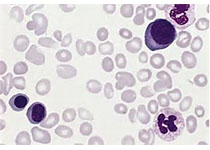
现有研究人员在C57BL/6背景下开发出一种转基因小鼠模型(Eμ-SOX11-EGFP),可在B细胞特异性IgH-Eμ增强子的控制下表达小鼠SOX11和EGFP。在B细胞中过表达SOX11表现为寡克隆B细胞在脾脏、骨髓和外周血中增生,免疫表型(CD5+CD19+CD23-)与人类MCL相同。
而且,对这些小鼠脾细胞进行磷酸-CyTOF分析显示,在BCR信号通路中,pBTK和其他分子过度激活;连续移植转基因供体的骨髓可导致潜伏期缩短而死亡。
综上所述,在B细胞中过表达SOX11可促进BCR信号,模拟人类MCL的疾病表型。
原始出处:
Pei-Yu Kuo,et al.SOX11 augments BCR signaling to drive MCL-like tumor development.2018 :blood-2018-02-832535; doi: https://doi.org/10.1182/blood-2018-02-832535
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肿瘤细胞#
30
学习了.谢谢分享
62
学习了.长知识
59