Adv Healthc Mater:开发出磁控干细胞用于肿瘤药物靶向输送
2017-01-05 佚名 生物谷
来自托木斯克理工大学(TPU)的科学家开发出了一种控制间充质干细胞(MSCs)的新技术,可以更有效治疗肿瘤。为了攻击肿瘤细胞,科学家们尝试采用磁场控制病人的自体细胞,因为自体细胞不会被机体免疫系统排斥,因此可以直接将药物带到肿瘤中心。这项新技术由TPU、巴普甫夫医科大学及伦敦大学女王学院的研究人员一起完成。 他们将约10微米的MSCs与包含药物的磁性微米颗粒结合在一起,采用外加磁场驱使细胞
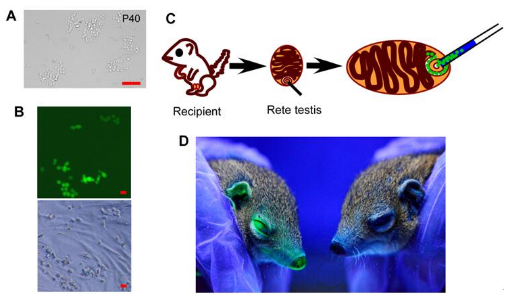
来自托木斯克理工大学(TPU)的科学家开发出了一种控制间充质干细胞(MSCs)的新技术,可以更有效治疗肿瘤。为了攻击肿瘤细胞,科学家们尝试采用磁场控制病人的自体细胞,因为自体细胞不会被机体免疫系统排斥,因此可以直接将药物带到肿瘤中心。这项新技术由TPU、巴普甫夫医科大学及伦敦大学女王学院的研究人员一起完成。
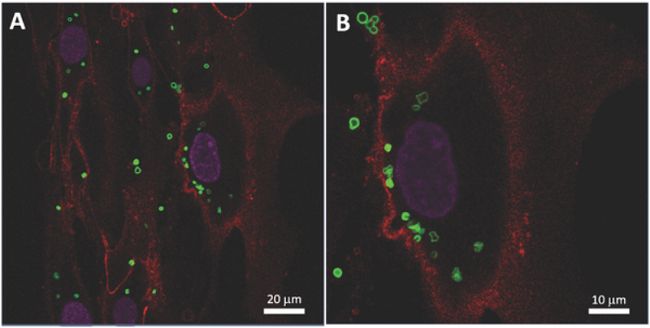
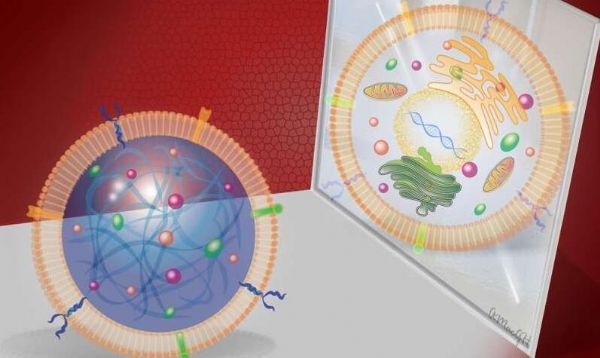
他们将约10微米的MSCs与包含药物的磁性微米颗粒结合在一起,采用外加磁场驱使细胞向肿瘤组织移动,到达肿瘤组织后这些微米颗粒会将包载的药物释放出来,因此药物被精准输送到肿瘤组织,不会对正常组织造成伤害。
“MSCs本身就具有肿瘤趋向性,它们还可以在体内外分化成为骨、脂肪、肌肉或结缔组织。因此MSCs在替代疗法、基因或细胞工程领域很具有吸引力。”共同作者之一Alexander Timin说道,他是TPU的一名研究员。
这也是研究人员第一次证明磁性微米颗粒可以与MSCs有效结合,可以此修饰细胞或者设计磁控细胞、组织工程系统等。
作者解释道:“值得注意的一点是MSCs可以高效结合磁性微米颗粒,同时毒性较小。由于微米颗粒被MSCs吞噬进入细胞内,我们就得到了一种新型细胞平台,它们可以对外加磁场产生响应形成含有数千个细胞的细胞球。同时,我们的结果表明这个平台可以创造下一代细胞工程产品,达到在体内高效靶向输送药物的目的。”
这项最新成果最近发表在《Advanced Healthcare Materials》上。
原始出处
Kirill V. Lepik et al,Mesenchymal Stem Cell Magnetization: Magnetic Multilayer Microcapsule Uptake, Toxicity, Impact on Functional Properties, and Perspectives for Magnetic Delivery, Advanced Healthcare Materials (2016).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ALT#
27
#药物靶向#
42
#肿瘤药物#
22
#肿瘤药#
35
#Health#
25