JAHA:早期冠状动脉粥样硬化和内皮功能障碍患者的血浆神经酰胺水平升高
2022-03-19 MedSci原创 MedSci原创
在没有心外膜冠状动脉疾病的情况下,循环神经酰胺水平升高与冠状动脉内皮功能障碍之间存在关联。这项研究支持血浆神经酰胺作为早期冠状动脉粥样硬化的潜在生物标志物或治疗靶点的作用。
早期冠状动脉粥样硬化的特征是冠状动脉内皮功能障碍(CED)。CED发生在心外膜动脉和随后调节心肌血液供应。血浆中神经酰胺水平升高是晚期心外膜冠状动脉疾病患者心血管疾病和死亡率的独立预测因子。然而,研究人员对早期心外膜冠状动脉疾病中血浆神经酰胺的水平变化及临床意义了解仍然有限。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员评估了血浆神经酰胺在以冠状动脉内皮功能障碍为特征的早期冠状动脉粥样硬化中的作用和意义。

研究人员在出现胸痛和非阻塞性心外膜冠状动脉疾病的参与者中测量了冠状动脉内皮功能。患者(n=90)用乙酰胆碱检测冠状动脉内皮功能是否存在异常(冠状动脉直径减少≥20%或冠状动脉血流增加≤50%)。
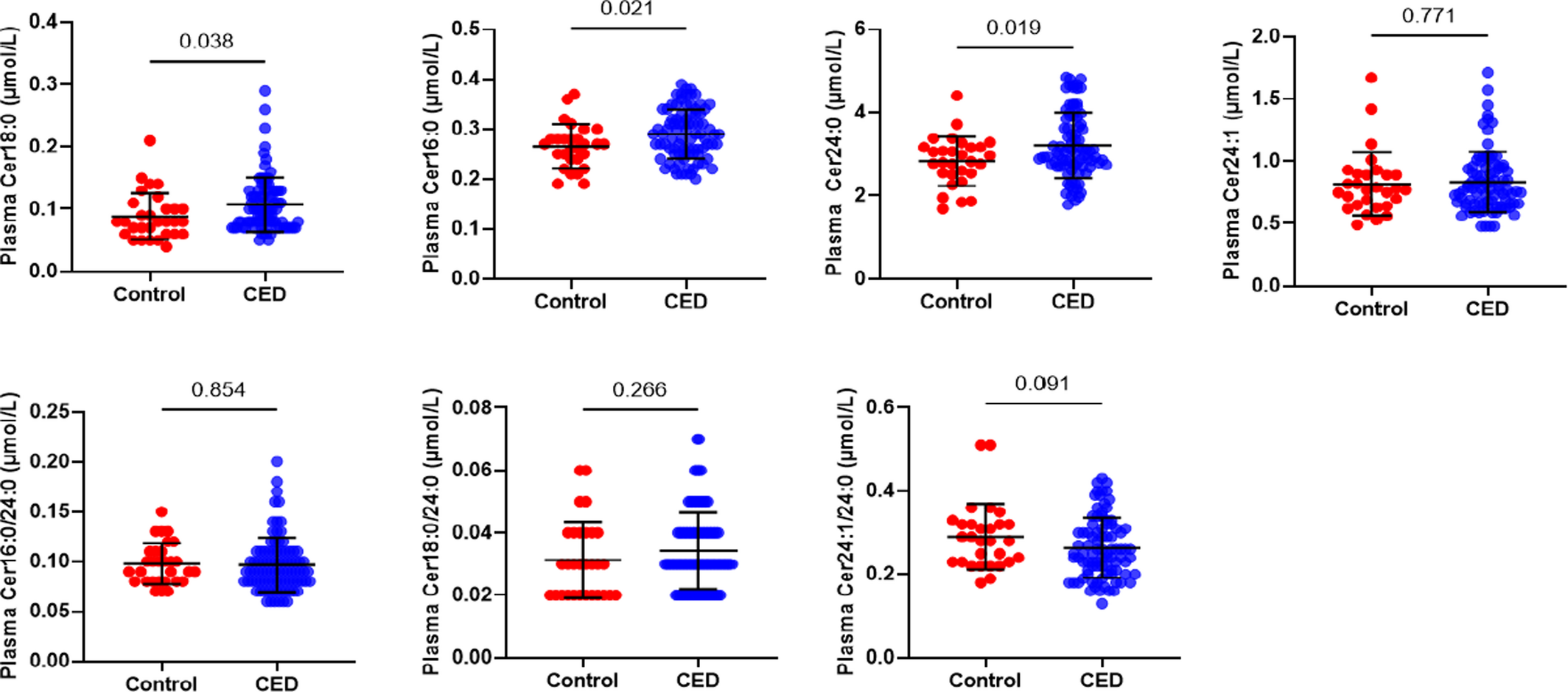
该研究共有30名对照者具有正常的冠状动脉内皮功能。冠状动脉内皮功能正常和异常的参与者血浆神经酰胺18:0(P=0.038)、16:0(P=0.021)和24:0(P=0.019)的浓度存在显著差异。神经酰胺24:0(比值比[OR]为2.23[95%CI为1.07-4.66];P=0.033)和16:0(OR为1.91×106[95%CI为11.93-3.07×1011];P=0.018)与冠状动脉内皮功能障碍独立相关。在患有内皮依赖性冠状动脉功能障碍的参与者(n=78)中,神经酰胺16:0(OR为5.17×105[95%CI为2.83-9.44×1010];P=0.033)、24:0(OR为2.98[95%CI为1.27-7.00];P=0.012)和24:1/24:0(OR为4.39×10−4[95%CI为4×10−7-0.48];P=0.030)浓度更有可能升高。
目前的研究表明,在没有心外膜冠状动脉疾病的情况下,循环神经酰胺水平升高与冠状动脉内皮功能障碍之间存在关联。这项研究支持血浆神经酰胺作为早期冠状动脉粥样硬化的潜在生物标志物或治疗靶点的作用。
原始出处:
Nadia Akhiyat.et al.Plasma Ceramide Levels Are Elevated in Patients With Early Coronary Atherosclerosis and Endothelial Dysfunction.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022852
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内皮功能障碍#
45
#粥样硬化#
31
#AHA#
43
#功能障碍#
33
#内皮功能#
52
#神经酰胺#
38