Orthop Surg:交锁髓内钉内固定治疗胫骨骨折术中识别胫骨远端冠状面畸形的回顾性研究
2022-09-22 医路坦克 MedSci原创
胫骨骨折在创伤骨科中很常见,其中大部分是高能量损伤,并伴有严重的软组织损伤。本文目的是开发一种新的方法,在闭合复位和髓内钉固定治疗胫骨骨折时,确定是否存在冠状面畸形(外翻和内翻)。
胫骨骨折在创伤骨科中很常见,其中大部分是高能量损伤,并伴有严重的软组织损伤。对于胫骨远端骨折的治疗缺乏共识,因为手术治疗需要确保稳定的固定,同时将手术入路和内固定对软组织的继发性损伤降至最低。良好的骨折复位和正确选择固定装置可能会提供更好的疗效。对于干骺端骨折或干-干连接处骨折,固定装置的选择和固定技术存在争议。在目前治疗胫骨骨折时,传统外固定架结合钢板内固定仍被认为是有效的固定方法。然而,有报道显示,由于髓内钉独特的血液供应和解剖特点,软组织出现了更多的并发症,包括针道感染、浅层或深层感染、伤口延迟愈合和软组织坏死,这导致髓内钉固定的应用越来越多,作为一种分担负荷的装置,使患者能够及早负重。
由于胫骨髓内钉固定对骨折周围软组织的干扰小,骨折愈合率高,已成为12-14岁移位胫骨骨折的标准治疗方法。研究指出,带锁髓内钉治疗胫骨骨折手术时间短,术后功能恢复好。然而,髓内钉固定仍然存在一些不足,如膝关节前疼痛。
本文目的是开发一种新的方法,在闭合复位和髓内钉固定治疗胫骨骨折时,确定是否存在冠状面畸形(外翻和内翻)。
方法:对2018年1月至2019年1月在我科创伤中心接受闭合复位髓内钉内固定治疗的33例胫骨骨折患者进行回顾性分析。33例患者中,男性23例,女性10例,年龄22-69岁,平均41岁。术前常规拍摄标准的正位和侧位X线片。术中通过标准进钉点插入胫骨髓内钉后,利用正后位X线片上远端水平交锁钉与胫距关节面间的平行关系,判断胫骨远端骨折是否发生外翻或内翻畸形。通过从损伤到手术的平均间隔、健侧和患侧的胫骨远端外侧角(LDTA)、并发症和Olerud-Molander踝关节评分来分析放射学和临床结果。结果:33例患者术后随访13-25个月,平均18.7个月。骨折愈合时间3-6个月,平均4.3个月。并发症发生率为60.6%(20例),其中深静脉血栓形成4例,感染及延迟愈合1例,轻、中度膝前痛15例。术后健侧LDTA测量值为87.3±0.00到89.6(平均88.7±0.8)。健侧与患侧比较差异无统计学意义(t=1.865,P=0.068)。术中测量显示外翻畸形6例,内翻畸形3例,所有畸形均在术中得到矫正。术后12个月按Olerud-Molander踝关节评分,优22例,良8例,可2例,差1例。
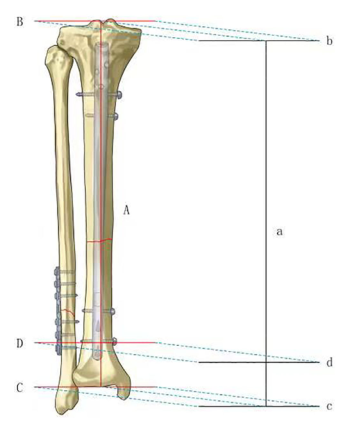
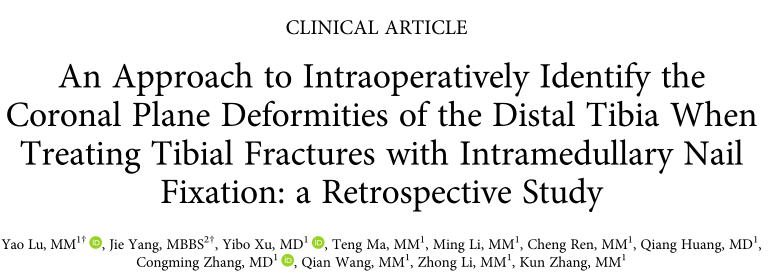
图1 冠状面上投影线的一般视图。胫骨髓内钉投影线(线a)、膝关节面投影线(线b)、胫距关节面投影线(线c)和远端水平交锁螺钉轴投影线(线d)。
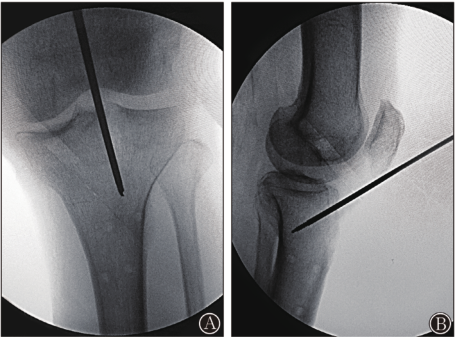
图2 髓内钉理想起点示意图。(A)术中AP视图上导丝的理想起点。(B)术中侧位视图上导丝的理想起点。
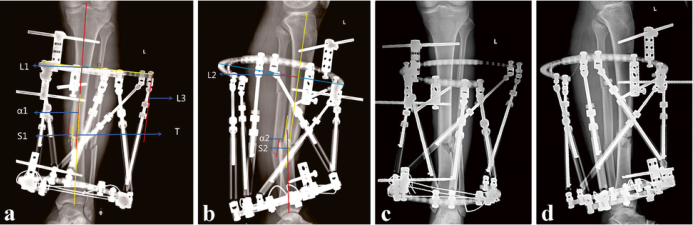
图3 一个典型病例,一名21岁男性经历了一次道路交通事故,导致左小腿和右膝盖疼痛,活动受限。急诊室的x光照片显示左侧胫骨和腓骨骨折合并对侧胫骨平台骨折。(A)左胫骨和腓骨骨折(AO/OTA 42-C3 ),如AP视图所示。(B)侧视图上左侧胫骨和腓骨骨折(42-C3)。(C)通过导丝插入手指缩小装置。(D)在逐渐扩髓后插入钉,远端交锁螺钉通过徒手操作锁定。c线和d线之间出现一个夹角,指向术中影像增强手绘图上的腓骨。(E)远端碎片的AP视图显示了外翻畸形。(F)在对远端胫骨碎片应用poller螺钉技术后,重新插入钉。(G)c线和don线图像增强和手绘示意图之间的平行关系表明术中矫正了外翻畸形。
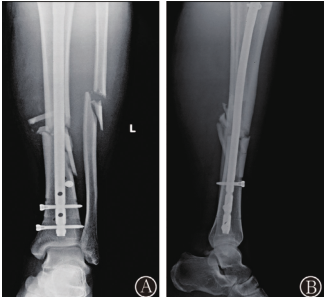
图4 术后影像学结果显示满意的复位、对齐和植入位置。(A)手术后2天的x光片的AP视图。(B)手术后2天的x光片侧视。

图5 手术后1年的功能结果。(A)1年随访时踝关节跖屈。(B)1年随访时踝关节的背屈。(C)1年随访时膝关节的活动范围。(D)术后1年随访时的AP片。(E)术后1年随访时的侧位片。
结论:术中正位X线片上胫距关节面与远端水平交锁钉的平行关系可确定胫骨远端髓内钉通过标准进钉后骨折区内翻或外翻的起始时间。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胫骨骨折#
48
#畸形#
0
#胫骨#
41
#髓内钉#
47
#内固定#
40
#回顾性研究#
41