J Pediatr:儿童功能性便秘行物理治疗能否改善其症状?
2021-05-25 MedSci原创 MedSci原创
儿童功能性便秘是一个世界性的常见问题,面临着令人尴尬的症状,包括腹痛、排便疼痛、大便和大便失禁。近日,一项随机试验中,研究人员探究了物理治疗联合常规治疗与单纯的常规治疗相比对荷兰4-17岁的儿童功能性
儿童功能性便秘是一个世界性的常见问题,面临着令人尴尬的症状,包括腹痛、排便疼痛、大便和大便失禁。近日,一项随机试验中,研究人员探究了物理治疗联合常规治疗与单纯的常规治疗相比对荷兰4-17岁的儿童功能性便秘的治疗效果,研究结果已发表于J Pediatr。
研究过程中,初级保健医生招募了被诊断为功能性便秘的儿童(n = 234),儿科医生招募了被诊断为功能性便秘的新转诊儿童(n = 11),随访8个月。常规治疗包括如厕训练、营养建议和泻药处方,而物理治疗则侧重于解决排便障碍问题。主要结果是8个月的治疗成功率,定义为没有功能性便秘而没有使用泻药。次要结果包括:无论是否继续使用泻药,都没有功能性便秘,以及整体感知的治疗效果。
对患儿进行随机分组,分别接受常规治疗联合物理治疗或常规治疗(每组67人),平均(SD)年龄为7.6(3.5)岁。意向治疗人群的纵向分析结果显示,在常规治疗的基础上增加物理治疗,治疗成功率并没有显著提高(校正后的相对风险[aRR] 0.80,95%CI 0.44-1.30)。在4个月时,接受物理治疗的儿童的治疗成功率(17%)低于仅接受常规治疗的儿童(28%),但到8个月时,两组治疗成功率相似(分别为42%和41%)。无论是否继续使用泻药,8个月内各组之间没有功能性便秘的儿童比例没有显著差异(aRR 1.12,95% CI 0.82-1.34)。值得注意的是,家长报告物理治疗后患儿的整体症状改善明显多于常规治疗(aRR 1.40;95% CI 1.00-1.73)。
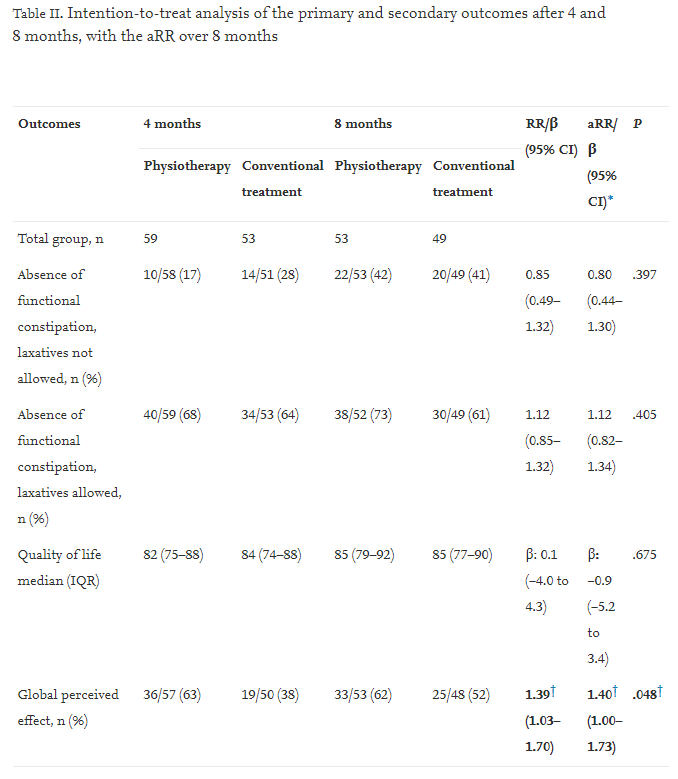
综上所述,该研究并没有发现任何证据可以推荐在初级保健中对所有患有功能性便秘的儿童进行物理治疗。
原始出处:
Jojanneke J G T van Summeren, et al., Physiotherapy for Children with Functional Constipation: A Pragmatic Randomized Controlled Trial in Primary Care. J Pediatr. 2020 Jan;216:25-31.e2. doi: 10.1016/j.jpeds.2019.09.048.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
29
#功能性便秘#
35
#PE#
38
#功能性#
36
学习了
61