PLOS Biol:研究将试验抗抑郁药治疗反应,使抑郁症得以正确治疗!
2017-12-30 枫丹白露 来宝网
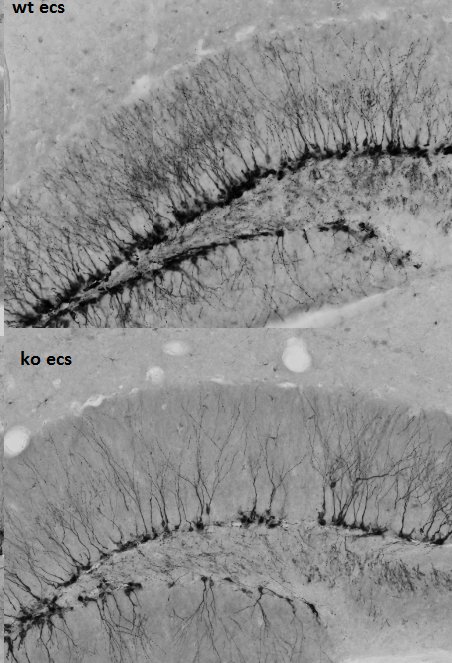
来自小鼠的新证据表明,为什么抗抑郁药治疗可以缓解一个人的抑郁症。这项研究于12月28日在开放获取期刊PLOS Biology上发表,由美因茨大学医学中心和马克斯普朗克精神病研究所的MarianneMüller和国际团队领导。研究人员开发了一个小鼠模型,使他们能够识别与抗抑郁药治疗反应有关的血液特征,并且可以显示压力相关的糖皮质激素受体在抑郁症康复中的重要性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑郁药#
37
#Biol#
35
#Bio#
38
学习一下谢谢分享
46
#抗抑郁#
45
一起学习学习
60
非常好.谢谢分享
62