OncoImmunology:超10万肿瘤患者大规模荟萃分析,再证TMB免疫治疗疗效预测价值!
2019-07-05 佚名 肿瘤资讯
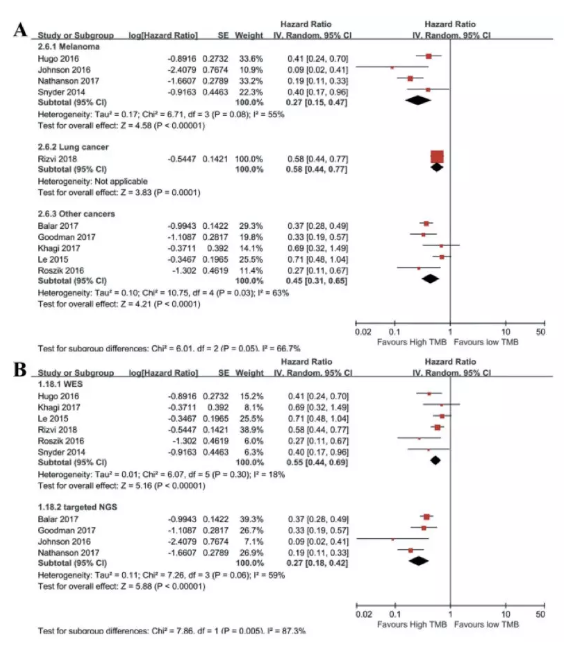
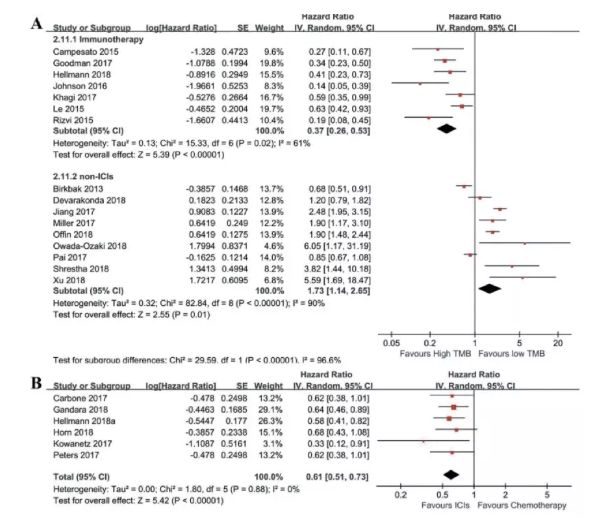
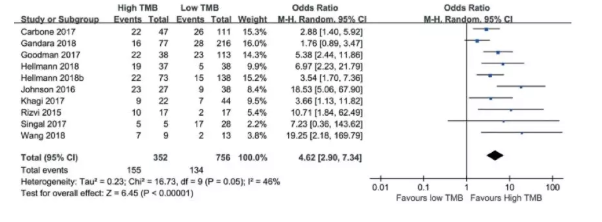
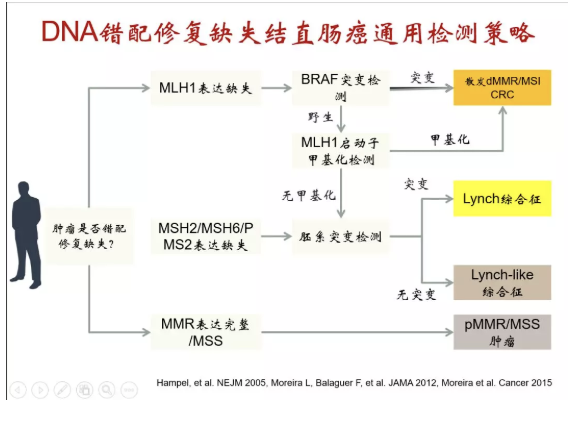
免疫检查点抑制剂的兴起大大改变了传统的肿瘤治疗策略,而程序性死亡受体-配体1(PD-L1)表达以及肿瘤突变负荷(TMB)等疗效预测标记物的发现,进一步提高了免疫药物的响应和获益。目前,TMB已从一个探索性预测标志物逐步走向FDA获批的伴随诊断,并被列入2019年NCCN指南。既往多项研究已探索了TMB与免疫治疗之间的关系,但在预测总生存(OS)或化疗预后方面,研究结果并不一致,颇具争议。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#荟萃分析#
36
#大规模#
0
#TMB#
44
#荟萃#
39
#肿瘤患者#
38
#预测价值#
35
谢谢梅斯提供这么好的信息,学到很多
46