Nature:科学家亲眼见证正常上皮细胞疯狂围剿癌基因突变细胞,把癌细胞扼杀在萌芽中
2017-08-14 王鑫英 BioTalker 奇点网
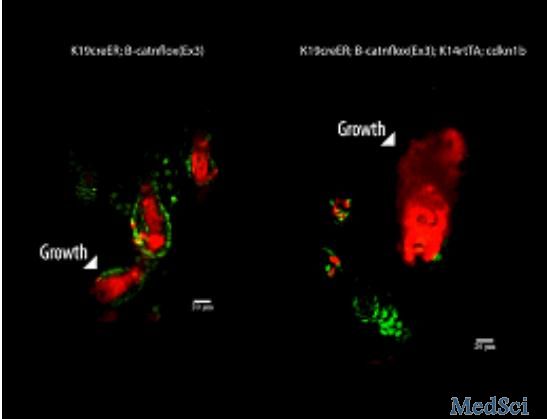
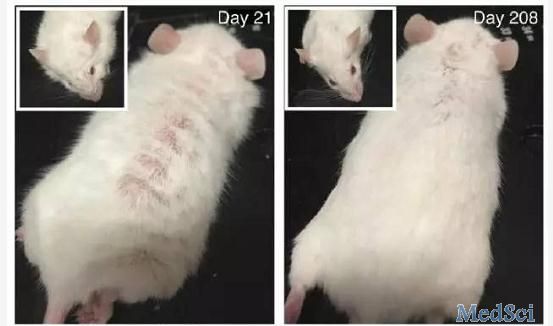
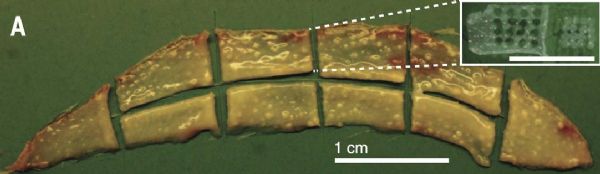
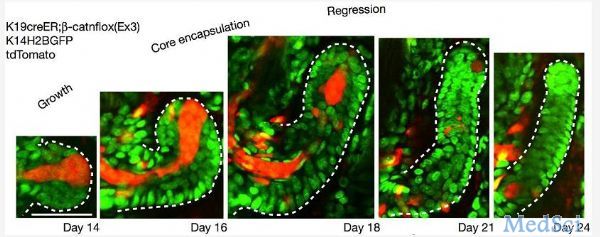
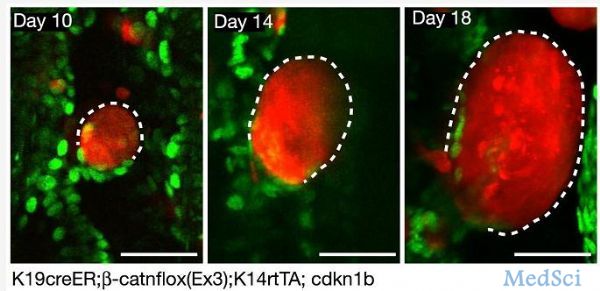
覆盖在人体皮肤和体内各种腔道(食管、胃、肠和气管等)表面的上皮细胞,是恶性肿瘤发生的主要部位,其中很重要的两个原因是:上皮细胞分裂比较活跃和上皮细胞受周围环境影响较大,这也导致上皮细胞发生基因突变的概率更高。




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
39
#突变细胞#
36
#疯狂#
37
#癌细胞#
35
#癌基因#
36
#上皮细胞#
27
不错的文章,值得学习。
60
学习一下知识
61