JACC:缓激肽受体B2基因附近的常见变异可增加ACEi相关血管性水肿风险
2021-08-16 Nebula MedSci原创
位于缓激肽受体 B2 基因附近的常见变异与 ACE 抑制剂相关血管性水肿的风险增加有关
血管性水肿是一种罕见、但潜在威及生命的与血管紧张素转换酶 (ACE) 抑制剂相关的不良反应。识别与此不良事件相关的潜在遗传因素可能有助于筛查高风险患者。
本研究目的是明确与 ACE 抑制剂相关的血管性水肿有关的遗传风险因素。
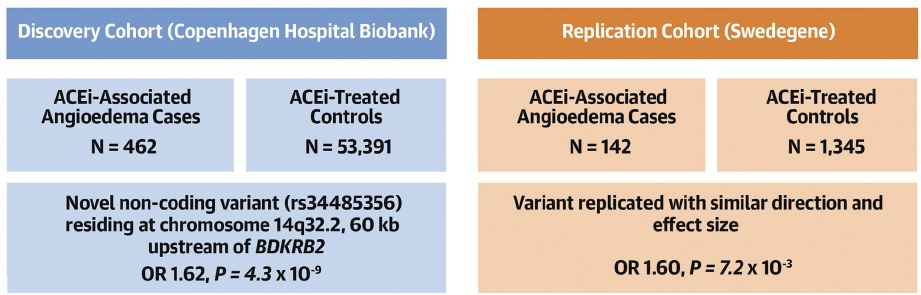
在服用 ACE 抑制剂的欧洲后裔患者中进行了一项全基因组关联研究,分为发现队列(哥本哈根医院生物样本库)和重复验证队列(Swedegene)。病例定义为在服用 ACE 抑制剂后 180 天内发生血管性水肿事件的受试者。对照组定义为持续接受 ACE 抑制剂治疗且无血管性水肿病史的患者。
发现队列共包含 462 例血管性水肿病例和53391位服用 ACE 抑制剂治疗的对照个体。重复验证队列包含 142 例病例和 1345 位采用 ACE 抑制剂治疗的对照个体。
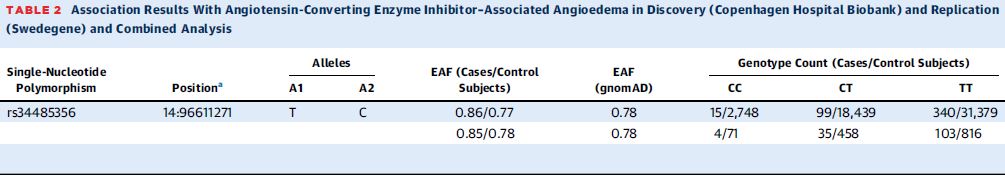
rs34485356位点的变异统计及与ACEi相关血管性水肿的相关性
在发现队列中,一个位于染色体 14q32.2 上的位点经鉴定与血管性水肿相关,全基因组显著性水平为 p<5×10-8。该位点的先导变异 rs34485356 是位于缓激肽受体 B2(BDKRB2 )上游 60 kb 的基因间变异(优势比[OR] 1.62;95%CI 1.38-1.90;p=4.3×10-9)。该变异在重复验证队列中得到了证实,具有相似的检测和效应大小(OR 1.60; 95%CI 1.13-2.25; p=7.2×10-3)。
此外,研究人员还发现,该风险等位基因的携带者的收缩压(-0.46 mmHg/T等位基因;95%CI -0.83~-0.10; p=0.013)和舒张压(-0.26 mmHg/T等位基因;95%CI -0.46~-0.05; p=0.013)明显更低。
总结示意图
总之,在这项关于 ACE 抑制剂治疗个体的全基因组关联研究中,研究人员发现,位于缓激肽受体 B2 基因附近的常见变异与 ACE 抑制剂相关血管性水肿的风险增加有关。
原始出处:
Jonas Ghouse, et al. Association of Variants Near the Bradykinin Receptor B2 Gene With Angioedema in Patients Taking ACE Inhibitors. J Am Coll Cardiol. 2021 Aug, 78 (7) 696–709
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
0
#血管性#
47
#ACE#
41
#ACC#
52
#水肿#
30
#变异#
30
#血管性水肿#
39
学习学习
58
学习学习
66
位于缓激肽受体 B2 基因附近的常见变异
58