Cell:miR-124可能成为肝癌治疗新靶标
2012-03-10 MedSci MedSci原创
近日来自美国哈佛医学院达纳法癌症研究所(Dana-Farber Cancer Institute)的研究人员通过小鼠模型发现了一种可触发肝脏炎症,促使正常细胞转化为癌细胞的分子机制,并证实一种特殊的micro-RNA——miR-124可用于预防和治疗肝癌。相关研究论文在线发表在12月9日的《细胞》(Cell)杂志上。[An HNF4α-miRNA Inflammatory Feedba
近日来自美国哈佛医学院达纳法癌症研究所(Dana-Farber Cancer Institute)的研究人员通过小鼠模型发现了一种可触发肝脏炎症,促使正常细胞转化为癌细胞的分子机制,并证实一种特殊的micro-RNA——miR-124可用于预防和治疗肝癌。相关研究论文在线发表在12月9日的《细胞》(Cell)杂志上。[An HNF4α-miRNA Inflammatory Feedback Circuit Regulates Hepatocellular Oncogenesis.Cell, Volume 147, Issue 6, 1233-1247, 9 December 2011]
文章来源:Cell. 2011 Dec 9;147(6):1233-47.
期刊影响因子:32.401
肝癌——全球第三大癌症死亡的原因——可由环境暴露或感染慢性肝炎引起,但迄今为止,人们对它们之间的联系知之甚少。
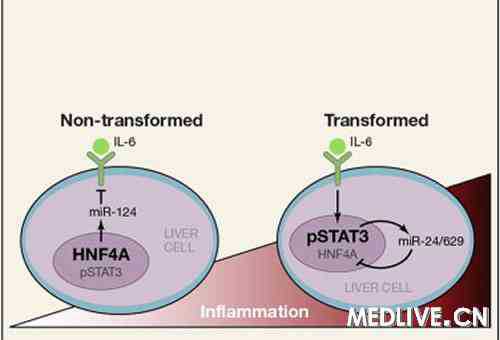
图 miR-124—HFN4α通路在肝细胞中
Iliopoulos和他的同事发现,小鼠接触致癌的化学物二乙基亚硝胺(DEN)后,通过活化分子电路,建立细胞炎症状态,最终形成肝癌。一旦这种炎症电路被打开,即使只需要短短几天时间,它就变成不可逆的,通过一个永无止境的反馈回路维持它的活性,Iliopoulos把它称为“雪球效应”。
Micro-RNAs是极其短的RNA,其作为一种信使分子帮助细胞根据DNA的指令构建蛋白,而不是翻译成蛋白。最近认为MiRNAs与人类疾病(包括各种癌症)的发病机制有关。达纳法伯小组发现miR-124和另一个反馈电路的关键控制因子HNF4α,在癌细胞中的活性下降。
HFN4α是生成肝细胞和维持它们正常生物功能的一个重要因子。Iliopoulos表示,当HNF4α被抑制,它制造细胞炎症的临时状态——癌症的前身。“仅在几天之后,通过这个持续放大的反馈电路,这种短暂的炎症应答转变成为一种慢性炎症应答,”他说。
由于HNF4α和miR-124互相作用,科学家假设促进miR-124活性可能会恢复HNF4α的正常活性,终止失控的炎症周期,让肿瘤停止生长。
为了验证这个想法,他们给予通过接触CEN患肝癌的小鼠体系miR-124,每周一次共四周。“我们发现miR-124抑制了超过80%的肿瘤生长速度和生长大小”,这种结果是通过诱发癌细胞自我毁灭实现的。同时,研究者们观察到,它对其他重要器官,如肾脏、脾脏、心脏和肺都没有毒性作用。
进一步地,他们表明给予miR-124的小鼠暴露在DEN下,事实上阻止了肝癌的发展。
“我们希望miR-124能够被用于具有潜在罹患肝癌的高风险人群,例如慢性丙型肝炎患者。或是作为肝癌患者的一种治疗剂,”Iliopoulos说。
文章编译自:Novel Therapeutic Approach for Liver Cancer Identified. ScienceDaily. 2011.12.9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#CEL#
19
#Cell#
18
#miR#
22
#肝癌治疗#
37
#靶标#
34