EJCB:抑制乳腺癌肿瘤细胞关键因子的揭示
2015-02-10 MedSci MedSci原创
一项由纽约爱因斯坦医学院的西班牙研究员何塞哈维尔•布拉沃 - 科尔德罗领导的新研究中,详细介绍了低表达前纤维蛋白-1的细胞如何在乳腺癌的肿瘤细胞中增加其转移并侵入其他组织的能力。 近年来,医学专家一直对开发新的治疗方法来对抗癌细胞的扩散非常感兴趣,癌细胞扩散也是癌症患者的最大的死亡原因。 然而,抑制或防止肿瘤细胞从原发肿瘤扩散的有效的治疗方法还没有被开发,其中关键一步就是肿瘤在转移过程中达到不
一项由纽约爱因斯坦医学院的西班牙研究员何塞哈维尔•布拉沃 - 科尔德罗领导的新研究中,详细介绍了低表达前纤维蛋白-1的细胞如何在乳腺癌的肿瘤细胞中增加其转移并侵入其他组织的能力。
近年来,医学专家一直对开发新的治疗方法来对抗癌细胞的扩散非常感兴趣,癌细胞扩散也是癌症患者的最大的死亡原因。
然而,抑制或防止肿瘤细胞从原发肿瘤扩散的有效的治疗方法还没有被开发,其中关键一步就是肿瘤在转移过程中达到不同的器官。
现在,由纽约艾伯特爱因斯坦医学院的一位西班牙研究员何塞哈维尔•布拉沃—科尔德罗领导领导的一项新研究发表在《欧洲细胞生物学》杂志上,并揭示了前纤维蛋白-1如何对肿瘤侵袭过程中形成确定结构进行干预。
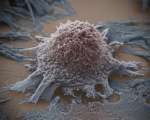
布拉沃—科尔德罗解释说:“为了达到这种有效程度,这些肿瘤细胞形成了一个称作侵袭伪足的亚细胞结构(从from the Latin invado, invade, and podio, feet; invasive feet),癌细胞借此来向机体的其他部分扩散。”
利用高分辨率显微镜技术,研究者研究了缺乏前纤维蛋白-1的肿瘤细胞的侵袭伪足的动力学,并描述了它们的作用和调节途径。
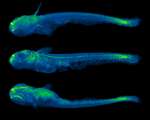
因此当乳腺癌肿瘤患者体内前纤维蛋白-1表达水平的下降和人乳腺癌肿瘤扩散到其他器官能力的增强息息相关。
这位西班牙的科学家描述说:“奇怪的是,与对照组细胞相比,缺乏前纤维蛋白-1的细胞显示的极强侵袭能力是通过侵袭伪足介导的。这就像我们已经采取了关闭制动系统,却失去对车辆的控制。”
更重要的是,布拉沃-科尔德罗补充说:“在前纤维蛋白-1不存在情况下,当细胞外基质降解时,侵袭伪足则表现为更为积极,并具有很强的侵入性的结构,这也解释了这些细胞的高转移潜能。”
一个关键结构
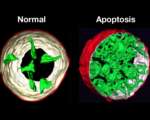
这项工作是与来自匹兹堡大学(宾夕法尼亚,美国)的研究人员合作完成的,研究表明了树突状伪足的内部结构和肌动蛋白细胞骨架(主要是真核细胞的脚手架)在它们的功能上的重要性,以及前纤维蛋白-1如何在调控中起着至关重要的作用。
专家指出:“如果我们破坏了脚手架,该结构就不能形成;如果我们以同样的方式有效的完成脚手架的组装,我们就可以形成具有更强侵袭力的组织。我们应该应用这些变量来抑制肿瘤的侵袭,让前纤维蛋白-1来调节这种平衡。”
研究者还描述了缺乏前纤维蛋白-1的细胞中能够让侵袭伪足有更强侵袭能力的分子途径。这个分子机制有效的在他们的成熟过程中起到了重要作用。
这项研究的主要作者、索诺拉州大学(墨西哥)亚历杭德拉•巴伦苏埃拉 - 伊格莱西亚斯声明:“这是一个成熟的问题。在缺乏这种蛋白质时侵袭伪足成熟更快,通过抑制前纤维蛋白-1的表达来迅速降解基质,因此,这些细胞具有更强的侵袭能力。”
目前研究人员强调:“所有的侵袭机制都是发现在亚细胞水平,我们确定了‘螺母和螺栓’的关系。我们必须调整以防止肿瘤细胞扩散。这将大大有助于开发抑制肿瘤转移过程的新治疗方法。”他们得出结论。
原始出处
A. Valenzuela-Iglesias, V.P. Sharma, B.T. Beaty, Z. Ding, L.E. Gutierrez-Millan, P. Roy, J.S. Condeelis, J.J. Bravo-Cordero. Profilin1 regulates invadopodium maturation in human breast cancer cells. European Journal of Cell Biology, 2014;
本文是MedSci编译,欢迎转载,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#关键因子#
38
非常好的文章,学习
117
很不错学习了
110
以阅
89
#肿瘤细胞#
27
Profilin1 主要调节invadopodium成熟,与乳腺癌侵犯有关
104