BMC: 老年人减少肉食摄入可降低NAFLD的风险!
2021-05-24 MedSci原创 MedSci原创
非酒精性脂肪性肝病(NAFLD)是与代谢综合征最相关的肝病,全球的患病率在25%左右,正成为全球主要的健康和经济负担。
非酒精性脂肪性肝病(NAFLD)是与代谢综合征最相关的肝病,全球的患病率在25%左右,正成为全球主要的健康和经济负担,此外,NAFLD不仅与肝脏疾病的不良结果相关,包括肝硬化和肝癌,而且还与非肝脏疾病的相关不良后果相关,如心血管疾病和糖尿病有关。有研究显示,不健康的生活方式会导致NAFLD风险增加,肉类消费量的增加会导致饮食中胆固醇,饱和脂肪和其他有害化合物的摄入量增加,这些与NAFLD密切相关。本研究旨在评估中老年人中肉食与NAFLD风险和肝脏相关生化指标的相关性。
研究人员对2015年4月至2017年8月在中国东南地区接受过身体检查的45岁以上的个体进行了回顾性研究。为了评估肉类摄入量与NAFLD风险之间的关联,研究人员采用logistic回归进行了相关性分析。用Spearman等级相关性检验了肉食与肝脏相关生化指标之间的关系。

本项研究结果显示高摄入量的红肉(> 71.00 g /天)与NAFLD风险增加呈正相关关系,吸烟,饮茶,体育锻炼减少以及患有高血压,血脂异常和糖尿病都是影响NAFLD的发病的危险因素。暴露-反应关系分析表明,摄入红肉与NAFLD风险呈正相关,而且研究人员发现红肉摄入量与肝脏的生化指标如:血清γ-谷氨酰转移酶,丙氨酸转氨酶,天冬氨酸转氨酶,总甘油三酯和高密度脂蛋白胆固醇水平显着相关。
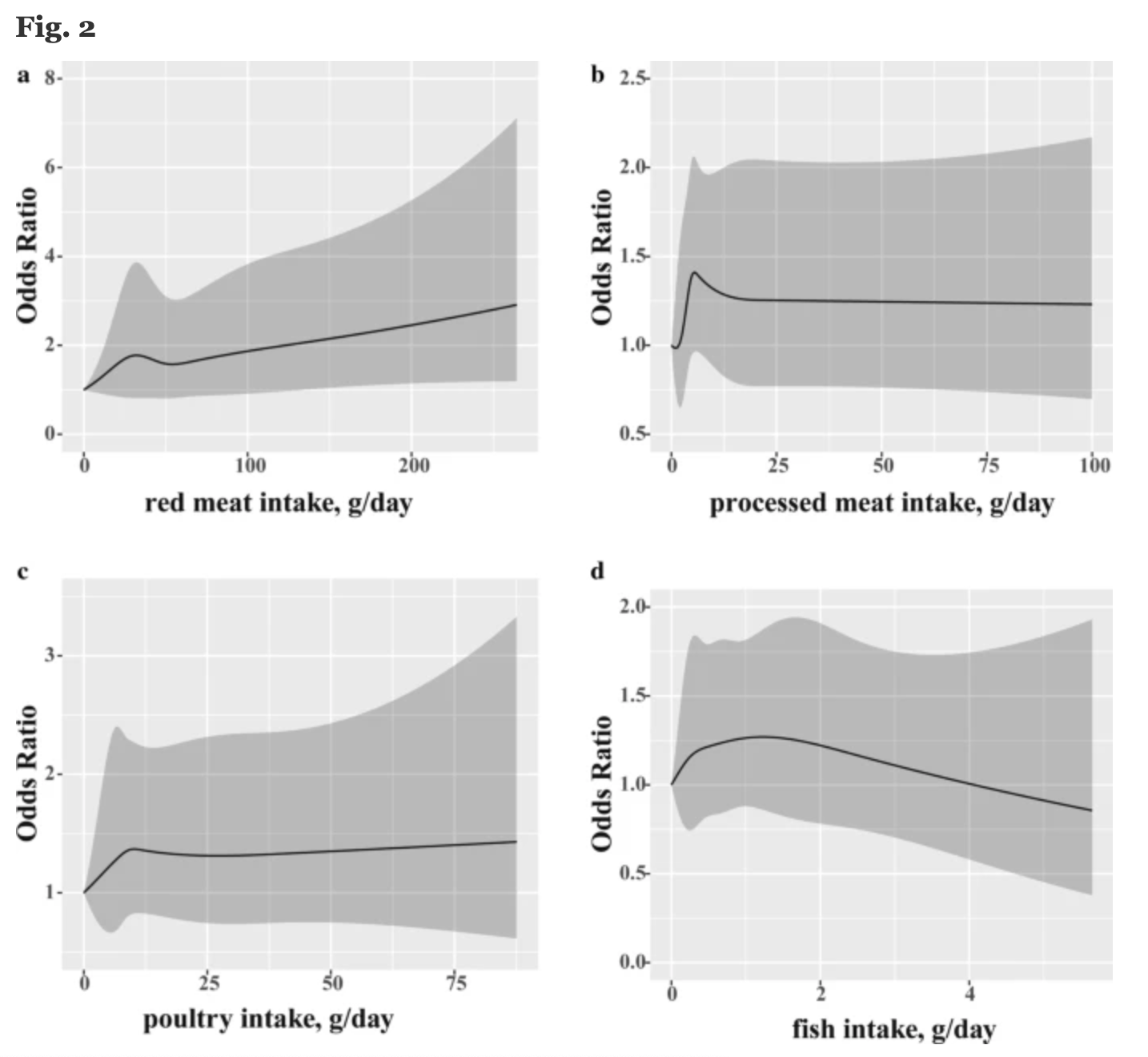
图:不同食物对于NAFLD的影响
本项研究证实大量食用红肉与NAFLD风险呈正相关关系。此外,血清中与肝脏相关的生化指标水平与红肉摄入量显着相关,减少肉食可以降低NAFLD的风险!
原始出处:
Hewei Peng. Et al. Association of meat consumption with NAFLD risk and liver-related biochemical indexes in older Chinese: a cross-sectional study.BMC Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMC#
32
#AFLD#
39
受教了
57
#学习#1
60