经桡动脉介入诊疗渐成主流
2010-09-20 MedSci原创 MedSci原创
作者:首都医科大学附属北京安贞医院 周玉杰 贾德安 图1 经桡动脉与经股动脉PCI示意图 图2 库利(Khoury)等研究表明,93%的冠状动脉疾病患者存在主动脉粥样硬化斑块,粥样硬化斑块主要分布在降主动脉(93%)和主动脉弓(80%),而较少分布于升主动脉(37%)。经桡动脉入路导管主要经过升主动脉,较少导致斑块破裂等并发症。 在2010年国际经桡
作者:首都医科大学附属北京安贞医院 周玉杰 贾德安
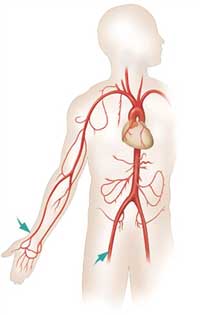
图1 经桡动脉与经股动脉PCI示意图
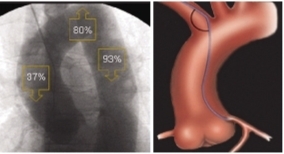
图2 库利(Khoury)等研究表明,93%的冠状动脉疾病患者存在主动脉粥样硬化斑块,粥样硬化斑块主要分布在降主动脉(93%)和主动脉弓(80%),而较少分布于升主动脉(37%)。经桡动脉入路导管主要经过升主动脉,较少导致斑块破裂等并发症。
在2010年国际经桡动脉介入治疗高峰论坛(TCI 2010)上,国内外专家就经桡动脉介入诊疗相关问题和技巧进行阐述,包括经桡动脉冠脉开口异常的介入治疗,桡动脉操作中常见的路径障碍及处理,以及如何经桡动脉完成旋磨技术、6F指引导管完成对吻扩张的技巧等。
来自日本的松景(Matsukage)教授介绍了Slender TRI的概念,主要是指通过减小指引导管的外径来减少外周血管并发症,减少对比剂用量,并获得更好的灵活性。由目前常用的6F导管过渡为4F、5F导管,可在临床上完成对70%病变的介入治疗。通过手法改变导引导管头端形态和曲度可明显增强支持力,并且完成复杂病变的介入治疗,更好地体现了微创治疗的理念。
会议邀请介入领域高水平专家作手术演示并通过卫星直播,使参会者同专家真正实现零距离接触,体会对各种病变处理的技巧与策略,开阔了眼界,拓宽了思路。在本次会议首设的“希望论坛”中,国内中青年术者带来了各自的精彩病例,包括对左主干病变、分叉病变、慢性完全闭塞(CTO)病变的处理方法,各种先进器械和技术的展示,以及各种并发症的应对策略,展示了我国介入界“新生代”医师的技术和实力。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好,为本人提供了一个学术发展的平台
130
#经桡动脉#
42
#桡动脉#
52
#介入诊疗#
0