J Bone Miner Res:地诺单抗停用后使用唑来膦酸盐治疗骨质疏松症的疗效
2021-06-30 MedSci原创 MedSci原创
地诺单抗的停用与骨质流失有关,并可能增加骨折风险。一项为期2年的随机、开放标签、干预性研究,研究人员调查了使用唑来膦酸钠(ZOL)治疗是否能防止骨质流失,以及ZOL的输注时间是否影响结果,研究结果已发
地诺单抗的停用与骨质流失有关,并可能增加骨折风险。一项为期2年的随机、开放标签、干预性研究,研究人员调查了使用唑来膦酸钠(ZOL)治疗是否能防止骨质流失,以及ZOL的输注时间是否影响结果,研究结果已发表于J Bone Miner Res。
研究纳入了61名骨质疏松症患者,在4.6±1.6年后停止使用地诺单抗。在最后一次注射地诺单抗后6个月(6M组,n = 20)或9个月(9M组,n = 20)或在骨转换率增加时(OBS组,n = 21)使用ZOL。使用DXA和骨转换标志物监测患者。主要终点是ZOL后6个月腰椎BMD(LSBMD)的变化以及未能保持BMD的患者比例。该研究正在进行(clinicaltrials.gov; NCT03087851)。
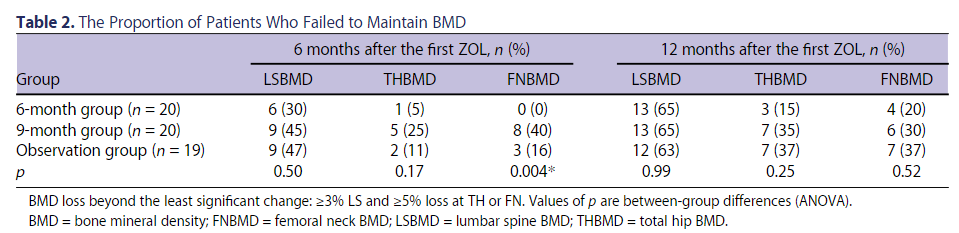
结果共纳入了61名参与者,59名患者在ZOL后12个月完成随访。ZOL后6个月,6M、9M和OBS组的LSBMD分别明显下降(平均值±SE)2.1%±0.9%、4.3%±1.1%和3.0%±1.1%;ZOL后12个月,6M、9M和OBS组分别下降4.8%±0.7%、4.1%±1.1%和4.7%±1.2%(P < .02,组间无差异)。在所有组别中,BMD的损失变化都最小;在脊柱处:6M组,n=6(30%);9M组,n=9(45%);和OBS组,n=9(47%);在全髋关节处:6M组,n=1(5%);9M组,n=5(25%);和OBS组,n=2(11%)。6M组的p-交联C端端肽(p-CTX)最初下降,但随后迅速增加,ZOL后6个月,p-CTX为0.60 ± 0.08 g/L。9M和OBS组的p-CTX迅速增加,被ZOL抑制,但随后再次增加;ZOL后6个月,9M和OBS组的p-CTX分别为0.47 ± 0.05 μg/L和0.47 ± 0.05 μg/L。9M组中有两名妇女出现了椎体骨折事件。
综上,该研究结果表明,无论什么时候用ZOL治疗,都不能完全防止停用地诺单抗的患者的BMD损失。
原始出处:
Anne Sophie Sølling, et al., Treatment with Zoledronate Subsequent to Denosumab in Osteoporosis: a Randomized Trial. J Bone Miner Res. 2020 Oct;35(10):1858-1870. doi: 10.1002/jbmr.4098.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Bone#
37
学习了
53
#唑来膦酸#
35
#骨质#
44
好文章
62
谢谢梅斯提供这么好的信息,学到很多
51