PNAS:慢性应激产生老年痴呆症相关的蛋白质聚集体
2012-04-10 mumu 生物谷
在3月26日网络版Proceedings of the National Academy of Sciences发表的文章中,加利福尼亚大学圣地亚哥医学院的研究人员指出,反复应激触发小鼠脑细胞内不溶性tau蛋白聚集体的生产和堆积。 聚合体类似于神经纤维缠结(NFTs),一种修改的蛋白质结构,是阿尔茨海默病的一种生理标志。该发现至少部分解释了临床研究为什么发现容易紧张的人与散发型阿尔茨海默氏病(A

在3月26日网络版Proceedings of the National Academy of Sciences发表的文章中,加利福尼亚大学圣地亚哥医学院的研究人员指出,反复应激触发小鼠脑细胞内不溶性tau蛋白聚集体的生产和堆积。
聚合体类似于神经纤维缠结(NFTs),一种修改的蛋白质结构,是阿尔茨海默病的一种生理标志。该发现至少部分解释了临床研究为什么发现容易紧张的人与散发型阿尔茨海默氏病(AD)发生之间的密切联系,其中散发型阿尔茨海默氏病占所有老年痴呆症病例的95%。
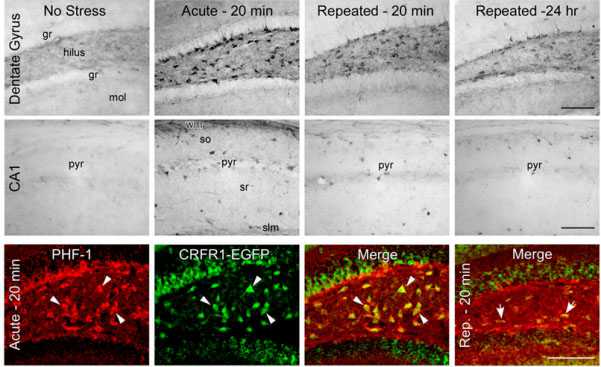
在小鼠模型中,研究人员发现,日常生活中可能经历的反复的情感应激事件导致神经元中tau蛋白质的磷酸化和可溶性改变,而这些事件对于阿尔茨海默氏病NFT病理学的发展是至关重要的。该作用在与记忆形成、组织和贮存相关的海马中最显著。在AD患者中,海马是典型的第一个受tau病理和大量细胞死亡与收缩重击影响的大脑区域。并不是所有形式的紧张都具有相同的威胁作用。既往研究指出,急性应激(单一的一过性事件)不会导致磷化tau蛋白累积上的持久性、逐渐减弱的长期变化。总体上,急性应激诱导的细胞改变是暂时的,可能是有益的。
急性应激可能对大脑可塑性有用,有助于易化学习。慢性应激和应激通路的连续激活可能导致形成应激回路的病理改变。人随着年龄增加,他们的神经回路也许激活得太多以致变得不再强健,也许不能从应激效应中完全复原。
研究发现,应激影响两个关键的促皮质释放素受体,意味着它们很可能是潜在治疗方法的靶标。我们不能排除应激,必需能对应激刺激有不同水平的反应。但可以用拮抗分子减少神经元的应激效应。应激系统还能反应,但是可调低大脑和海马的反应,以便不形成有害的永久性损伤。(生物谷bioon.com)

doi:10.1073/pnas.1203140109
PMC:
PMID:
Corticotropin-releasing factor receptor-dependent effects of repeated stress on tau phosphorylation, solubility, and aggregation
Robert A. Rissman, Michael A. Staup, Allyson Roe Lee, Nicholas J. Justice, Kenner C. Rice, Wylie Vale, and Paul E. Sawchenko
Exposure and/or sensitivity to stress have been implicated as conferring risk for development of Alzheimer's disease (AD). Although the basis for such a link remains unclear, we previously reported differential involvement of corticotropin-releasing factor receptor (CRFR) 1 and 2 in acute stress-induced tau phosphorylation (tau-P) and solubility in the hippocampus. Here we examined the role of CRFRs in tau-P induced by repeated stress and the structural manifestations of altered tau solubility. Robust tau-P responses were seen in WT and CRFR2 null mice exposed to repeated stress, which were sustained at even 24 h after the final stress exposure. A portion of phosphorylated tau in these mice was sequestered in detergent-soluble cellular fractions. In contrast, CRFR1 and CRFR double-KO mice did not exhibit repeated stress-induced alterations in tau-P or solubility. Similarly, treatment with CRFR1 antagonist attenuated repeated stress-induced tau-P. Using histochemical approaches in a transgenic CRFR1 reporter mouse line, we found substantial overlap between hippocampal CRFR1 expression and cells positive for phosphorylated tau after exposure to repeated stress. Ultrastructural analysis of negatively stained extracts from WT and CRFR2 null mice identified globular aggregates that displayed positive immunogold labeling for tau-P, as well as conformational changes in tau (MC1) seen in early AD. Given that repeated stress exposure results in chronic increases in hippocampal tau-P and its sequestration in an insoluble (and potentially prepathogenic) form, our data may define a link between stress and an AD-related pathogenic mechanism.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#慢性应激#
49
#痴呆症#
45
#白质#
45
#PNAS#
42
#蛋白质#
52
#应激#
43