NEJM:Daprodustat治疗接受透析的慢性肾病贫血
2021-12-16 MedSci原创 MedSci原创
在接受透析的CKD患者中,Daprodustat在提高血红蛋白水平和心血管结局方面与促红细胞生成剂相当
大多数正在接受透析治疗的慢性肾病(CKD)患者伴有贫血,导致患者生活质量降低、频繁输血和心血管事件风险升高。先前研究发现,传统的促红细胞生成剂(ESAs)治疗与患者心血管事件风险增加相关,而重组的人红细胞生成素及其衍生物可能增加患者中风、心肌梗死、血栓以及肿瘤风险。Daprodustat是一种口服缺氧诱导因子脯氨酰羟化酶抑制剂(HIF-PHIs),有研究发现其在提高血红蛋白水平方面的效果与ESAs相当。近日研究人员考察了Daprodustat对正在接受透析的CKD贫血患者的疗效及安全性。

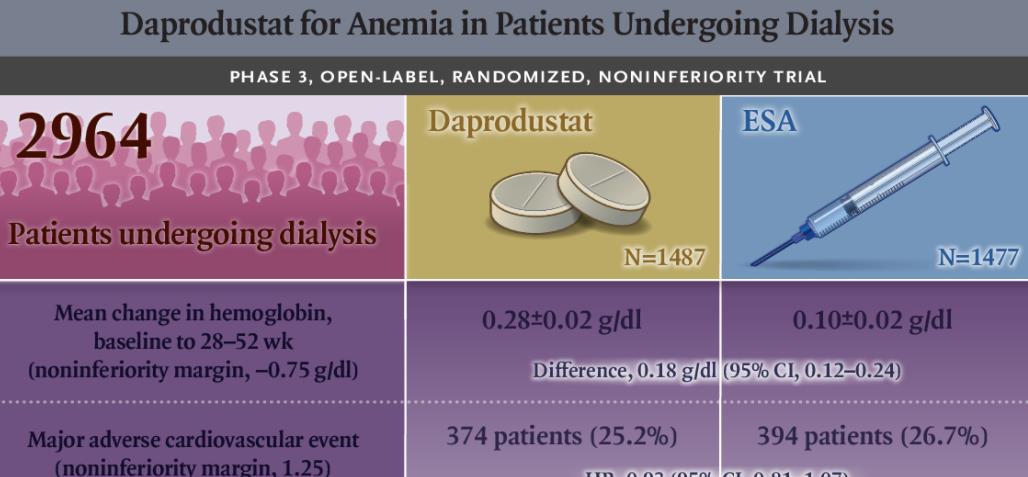
在这项随机、公开第3阶段试验中,正在接受透析且血红蛋白水平为8.0至11.5 g/分升的CKD患者随机接受Daprodustat或注射ESAs(血液透析患者接受epoetin alfa,腹膜透析患者接受阿法达贝汀)。研究的主要终点为从基线检查到第28-52周血红蛋白水平的平均变化和首次发生重大心血管不良事件(任何原因死亡、非致命性心肌梗死或非致命性中风的综合)。
2964名患者参与研究,基线平均血红蛋白水平为10.4g/分升。Daprodustat组从基线检查到第28周到第52周的血红蛋白水平的平均变化为0.28 g/分升,ESA组为0.10 g/分升(差异,0.18 g/分升),符合预先规定的非劣效性范围。在2.5年的中位随访期间,Daprodustat组1487名患者中有374名(25.2%)发生重大心血管不良事件,ESA组1477名患者中有394名(26.7%,危险比为0.9),符预先规定的非劣效性范围。组间其他不良事件率相似。
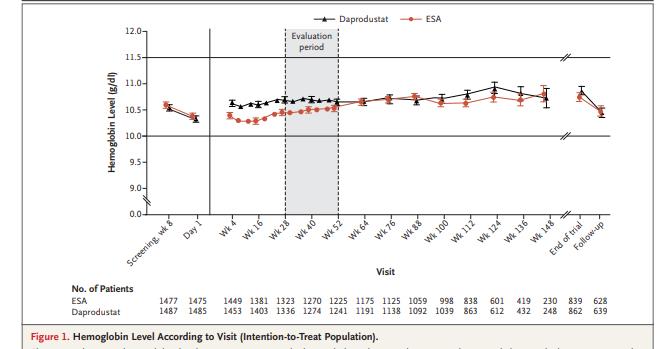
组间血红蛋白水平变化
在接受透析的CKD患者中,Daprodustat在提高血红蛋白水平和心血管结局方面与促红细胞生成剂相当。
原始出处:
Ajay K. Singh et al. Daprodustat for the Treatment of Anemia in Patients Undergoing Dialysis. N Engl J Med,December 16,2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#daprodustat#
51
学习了!
54
#PRO#
42
超好
57
多数正在接受透析治疗的慢性肾病(CKD)
0
学习了
69
认真学习了。
60