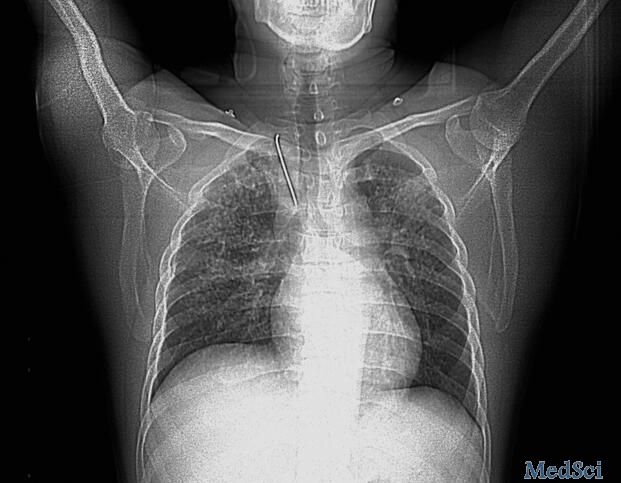
锁骨内固定钢钉脱落损伤主动脉 后果很严重
2017-08-21 佚名 环球医学
42岁男性患者急性起病,以恶心、呕吐伴喘憋为主要症状,同时伴大便失禁,为黄色稀便,呕吐物每次均为少量胃内容物及少量咖啡色物,无腹痛。患者血压低,心率快。但是抑酸、补液等治疗后患者病情继续加重,患者心率150次/分,呼吸困难,不能平卧,血压110/90mmHg。双肺满布湿啰音。表现出明显心力衰竭症状。面对不典型症状,怎么办?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#锁骨内#
46
学习了先进的技术水平
71
#损伤#
37
#主动脉#
44
#锁骨#
42
#内固定#
43
有点意思.谢谢分享
68
这个不错哦学习了
64
不错的.学习了.谢谢分享!
73