ImmunoGen的抗体 - 药物偶联物Mirvetuximab soravtansine未达到III期卵巢癌研究的主要终点
2019-03-02 不详 网络
ImmunoGen周五宣布,针对叶酸受体(FR)α阳性、铂类抗性卵巢癌患者的实验性抗体 - 药物偶联物(ADC)Mirvetuximab soravtansine的III期研究未能达到其无进展生存期(PFS)的主要终点。
ImmunoGen周五宣布,针对叶酸受体(FR)α阳性、铂类抗性卵巢癌患者的实验性抗体 - 药物偶联物(ADC)Mirvetuximab soravtansine的III期研究未能达到其无进展生存期(PFS)的主要终点。
FORWARD试验随机分配了366名患有FRα阳性、铂类抗性卵巢癌的患者以接受Mirvetuximab soravtansine或医生选择的单药化疗。结果显示,在整个研究人群中,Mirvetuximab soravtansine与化疗之间的PFS或总生存率的主要终点没有显著差异,尽管两组中确认的总体反应率(ORR)分别为22%和12%。同时,在具有高FRα表达的患者子集(占研究人群的60%)中,与化疗相比,接受Mirvetuximab soravtansine的患者的PFS更长,风险比为0.69。
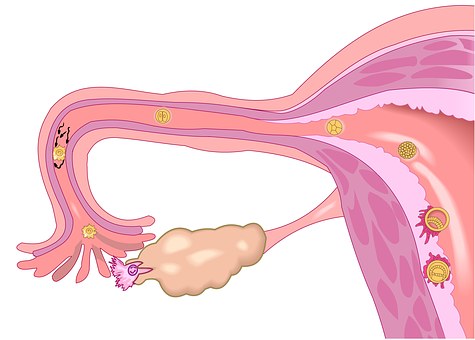
卵巢癌是发源自女性卵巢的癌症,会产生会入侵以及转移到其他部位的异常细胞。卵巢癌初期症状不明显,随病情进展,才会出现许多癌症的典型症状,包括胀气、腹胀、骨盆痛等。癌症较容易扩散到腹膜、淋巴结、肺脏、肝脏等部位。
原始出处:
http://www.firstwordpharma.com/node/1627538#axzz5gyg9tTzO
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
34
#III#
29
#主要终点#
37
#miR#
29
#III期#
33