Nat Commun:重大发现!一种肺癌亚型或能转化成为另一种亚型!
2017-04-18 生物谷 生物谷
日前,一项刊登在国际杂志Nature Communications上的研究研究报告中,来自肯塔基大学的研究人员通过研究发现,在特定的遗传状况下,一种非小细胞肺癌或许或转变成为另外一种肺癌亚型。 肺癌的谱系开关会对一些癌症疗法产生耐药性,这项研究中,研究人员具体检测了这种谱系开关发生的机制。此
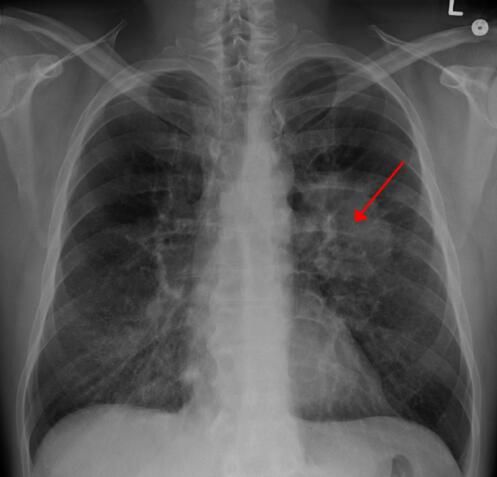
图片来源:medicalxpress.com
日前,一项刊登在国际杂志Nature Communications上的研究研究报告中,来自肯塔基大学的研究人员通过研究发现,在特定的遗传状况下,一种非小细胞肺癌或许或转变成为另外一种肺癌亚型。
肺癌的谱系开关会对一些癌症疗法产生耐药性,这项研究中,研究人员具体检测了这种谱系开关发生的机制。此前研究中,研究人员并不清楚成年人肺部中哪种细胞是引发非小细胞肺癌两种主要亚型的细胞起源,这两种主要的肺癌亚型分别为腺癌和鳞状细胞癌;同样地,研究人员也并不清楚这种不同肺癌亚型之间DNA组装的差异所在。肺部腺癌的存在在临床上被定义为所有腺癌病变都存在,而且相同的肿瘤中会出现鳞状损伤的明显分层,这就表明,肺腺癌和鳞状细胞癌或许来自于肺部组织中相同的细胞,但目前研究人员缺乏明确的证据来对此进行证实。
这项研究中,研究者发现,肺腺癌细胞能够以特殊的方式对DNA进行重新组装来转化成为肺部鳞状细胞癌,通过对腺癌肺部肿瘤的小鼠模型进行研究,研究人员将其同人类腺癌肺部肿瘤进行了对比证实了这种遗传性所在,人类的腺癌肺部肿瘤同小鼠在遗传性上相同,其中包括癌基因KRAS的激活以及肿瘤抑制自Lkb1的剔除;随后研究人员进行移植试验发现,在小鼠机体中,已经建立的肺部腺癌肿瘤能够过渡成为肺部鳞状细胞癌。
随后研究人员分离到了不同的肺部细胞,研究表明,仅有特定的肺部细胞能够产生具有谱系开关特性的肺部肿瘤。研究者Christine Fillmore Brainson教授表示,本文研究数据让我们非常激动,我们发现肺部组织中的细胞能够产生腺癌肿瘤,同时我们所利用的转化分离细胞的技术也能够应用于多种肺癌魔性的深入研究中。当EGFR酪氨酸激酶抑制剂疗法失败后,很多肿瘤学家观察到了谱系开关的存在,这种疗法在临床上往往会进行第二活检,然而通常在化疗后第二活检往往无法进行,研究者认为这种实践或许能够修订我们对化疗耐受性具体机制的理解。
最后研究者Brainson指出,如今我们阐明了谱系开关的分子机制,我们也将开始深入探究如何操控这种机制来开发出治疗肺癌的新型个体化疗法。
原始出处:
Haikuo Zhang, Christine Fillmore Brainson, n1, Shohei Koyama, et al. Lkb1 inactivation drives lung cancer lineage switching governed by Polycomb Repressive Complex 2. Nature Communications(2017),doi:10.1038/ncomms14922.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
0
#肺癌亚型#
34
#重大发现#
39
#Nat#
0
有意思的发现~
76