NEJM:用于晚期ALK阳性肺癌:劳拉替尼 or 克唑替尼
2020-11-19 MedSci原创 MedSci原创
涉及间变性淋巴瘤激酶(ALK)基因的染色体重排定义了对小分子ALK酪氨酸激酶抑制剂高度敏感的非小细胞肺癌(NSCLC)。过去有试验表明,第一代ALK抑制剂克唑替尼的功效优于
涉及间变性淋巴瘤激酶(ALK)基因的染色体重排定义了对小分子ALK酪氨酸激酶抑制剂高度敏感的非小细胞肺癌(NSCLC)。过去有试验表明,第一代ALK抑制剂克唑替尼的功效优于铂培美曲塞化疗,正是这一发现将克唑替尼确立为晚期ALK阳性NSCLC的标准一线治疗药物。 随后,一些随机的3期研究表明,第二代ALK抑制剂(包括艾来替尼,布里亚替尼和恩沙替尼)的功效又更优于克唑替尼。 这些发现导致第二代抑制剂替代了克唑替尼作为新的标准一线治疗药物。 然而,尽管第二代抑制剂的功效有所提升,但因其耐药性和复发性疾病(包括中枢神经系统疾病)导致疾病和死亡的副作用却始终无法得到缓解。

劳拉替尼是一种新型的第三代ALK抑制剂,在已进行的生化和细胞分析中表现出了比二代抑制剂更有效的作用,同时能够覆盖最大范围的ALK耐药性突变。劳拉替尼被设计成可穿越血脑屏障,其目的是为了达到在CNS中的高水平暴露。在第1和第2期研究中,劳拉替尼在先前的ALK抑制剂(第一代,第二代或两者)失败后仍具有有效的抗肿瘤活性。劳拉替尼在先前接受过基线中枢神经系统疾病(包括软脑膜疾病)治疗的患者中具有明显的颅内活性。考虑其功效和安全性,劳拉替尼是一种或多种ALK抑制剂无效的ALK阳性患者的标准治疗选择。
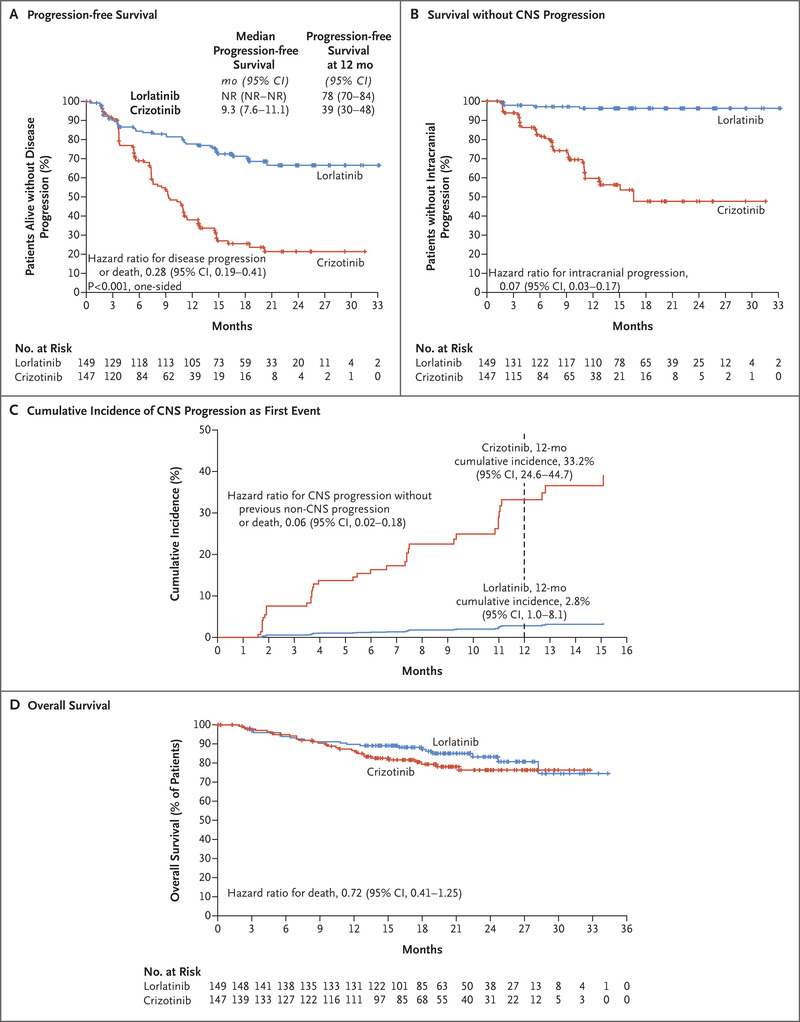
CROWN试验是一项全球性的随机3期试验,该试验比较了劳拉替尼与克唑替尼(试验开始时均按标准一线治疗)在先前未接受治疗的晚期ALK阳性NSCLC患者中的情况。研究人员进行了一项全球性的随机3期试验,对296名晚期ALK阳性NSCLC患者(未曾接受过全身性转移病治疗)进行了劳拉替尼与克唑替尼的疗效比较。主要终点是无进展生存,这是通过盲法独立中央评价评估的。 次要终点包括独立评估的客观反应和颅内反应。
在177例疾病进展或死亡的预期事件中有133例(75%)发生后,计划进行中期疗效分析。
劳拉替尼组在12个月时没有疾病进展的存活患者百分比为78%(95%置信区间[CI]为70至84),克唑替尼组为39%(95%CI为30至48)( 疾病进展或死亡的危险比为0.28; 95%CI为0.19至0.41; P <0.001)。 劳拉替尼组76%(95%CI,68至83)的患者和克唑替尼组58%(95%CI,49至66)的患者发生了客观反应。 在具有可测量的脑转移的患者中,分别有82%(95%CI,57至96)和23%(95%CI,5至54)发生了颅内反应,接受劳拉替尼的患者中有71%发生了颅内反应。 劳拉替尼最常见的不良事件是高脂血症,水肿,体重增加,周围神经病变和认知作用。 与克唑替尼相比,劳拉替尼与3级或4级不良事件(主要是血脂水平改变)的相关性更高(分别为72%和56%)。 因不良事件而中断治疗的患者分别占7%和9%。在对先前未经治疗的晚期ALK阳性NSCLC患者进行的结果中期分析中,与接受克唑替尼治疗的患者相比,接受劳拉替尼治疗的患者的无进展生存期更长,颅内反应频率更高。 但由于血脂水平的变化,劳拉替尼3级或4级不良事件的发生率比克唑替尼更高。
总体而言,劳拉替尼的安全性与以前的研究相似,而与其他ALK抑制剂相比,劳拉替尼具有明显的副作用。 在接受劳拉替尼的患者中,认知反应的报道率为21%,情绪副作用的报道为16%,这些副作用主要是低度的。认知和情绪变化通常出现在劳拉替尼给药后的前两个月内,并可通过剂量中断和减少来控制副反应的程度。体重增加则是由于食欲增加的原因,这是接受劳拉替尼治疗的患者的普遍报道。 认知和情绪变化可能是由于中枢神经系统中原肌球蛋白受体激酶B的脱靶抑制所致。与克唑替尼相比,劳拉替尼发生3或4级不良事件的频率更高(分别为72%和56%)。 但是,劳拉替尼组3级或4级不良事件的一半以上是胆固醇、甘油三酯或两者的升高。 高胆固醇血症和高甘油三酯血症是劳拉替尼报告的最常见的不良反应。 同样,劳拉替尼第3级或更高的不良事件发生率高于克唑替尼(73%比61%),而艾乐替尼的3级或更高的不良事件发生率比克唑替尼略低(45%比51%)。尽管劳拉替尼3级或4级不良事件的发生率较高,两组因不良事件而终止治疗的情况却是相似的(接受劳拉替尼的患者为7%,接受克唑替尼的患者为9%)。患者结局的报告也支持了劳拉替尼相对于克唑替尼的更为安全,生活质量也显著增高。
原始出处:
https://www.nejm.org/doi/full/10.1056/NEJMoa2027187?query=featured_home
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习
37
#ALK阳性#
40
涉及间变性淋巴瘤激酶(ALK)基因的染色体重排定义了对小分子ALK酪氨酸激酶抑制剂高度敏感的非小细胞肺癌(NSCLC)。
73
学习了
67
对学习学习
75
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
46