Heart:经导管主动脉瓣置入术后肾素-血管紧张素系统阻断治疗效果如何?
2017-10-24 xing.T MedSci原创
术后RAS阻断治疗与左室质量指数的逆转有关,并且降低了全因死亡率。这些数据需要通过前瞻性随机对照结果试验来进一步予以证实。
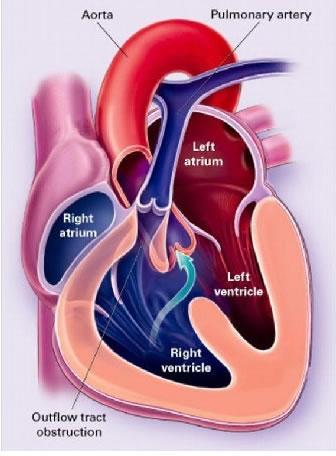
主动脉瓣狭窄患者接受经导管主动脉瓣植入术(TAVI)后持续的左心室肥厚(LV)与临床预后较差有关。然而,TAVI后最佳的药物治疗仍然未知的。近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员分析了肾素血管紧张素系统(RAS)阻断疗法对接受TAVI治疗的患者左心室肥厚和死亡率的影响。
在2013年10月至2016年4月之间,1215例接受TAVI治疗的患者被纳入优化的导管瓣膜干预(OCEAN)-TAVI登记中心。这个队列中的受试者根据术后RAS阻断剂治疗所使用的血管紧张素转换酶(ACE)抑制剂或血管紧张素受体阻滞剂(ARBs)来进行分层。RAS阻断组患者(n=371)在TAVI术后180天至少接受了一种处方药治疗,至少随访6个月,而那些没有服用任何ACE抑制剂或ARBs治疗的TAVI术后患者被列入无RAS阻断组(n=189)。
在术后6个月期间,阻断RAS组较无RAS阻断剂组左室质量指数逆转更大(-9±24% vs. -2±25%,P=0.024)。Kaplan Meier分析显示RAS阻断组累积的2年死亡率明显低于无RAS阻断组(7.5% vs. 12.5%;对数秩检验P=0.031)。调整混杂因素后,RAS阻断治疗与全因死亡率显著降低相关(风险比为0.45;95%可信区间为0.22-0.91;P=0.025)。
由此可见,术后RAS阻断治疗与左室质量指数的逆转有关,并且降低了全因死亡率。这些数据需要通过前瞻性随机对照结果试验来进一步予以证实。
原始出处:
Tomoki Ochiai,et al. Renin–angiotensin system blockade therapy after transcatheter aortic valve implantation. Heart. 2017.http://dx.doi.org/10.1136/heartjnl-2017-311738
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#置入术#
50
#阻断#
30
#肾素-血管紧张素系统#
38
#治疗效果#
35
#血管紧张素系统#
57
#主动脉瓣#
30
#ART#
30
#主动脉#
38
#经导管#
26
#经导管主动脉瓣置入术#
53