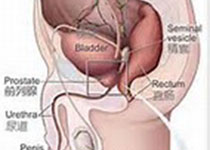
Int J Cancer:前列腺癌 vs 乳腺癌的发病率和死亡率表明,前列腺癌正在被过度诊断
2017-08-31 MedSci MedSci原创
全球乳腺癌发病率自20世纪70年代末开始一直呈上升趋势。美国8名妇女一生中就会有1人患乳腺癌。中国不是乳腺癌的高发国家,但不宜乐观,近年我国乳腺癌发病率的增长速度却高出高发国家1~2个百分点。2012年我国肿瘤登记地区前列腺癌发病率为9.92/10万,列男性恶性肿瘤发病率的第6位。发病年龄在55岁前处于较低水平,55岁后逐渐升高,发病率随着年龄的增长而增长,高峰年龄是70~80岁。家族遗传型前列腺
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发病率#
36
学习了谢谢分享
76
学习了谢谢分享
66
学习了.谢谢分享
74
学习了很有用
63
学习了
52
不错的文章.值得一读
23