张新军教授:从ACP/AAFP指南看老年高血压治疗策略
2017-09-25 陈年老刘 医学界心血管频道
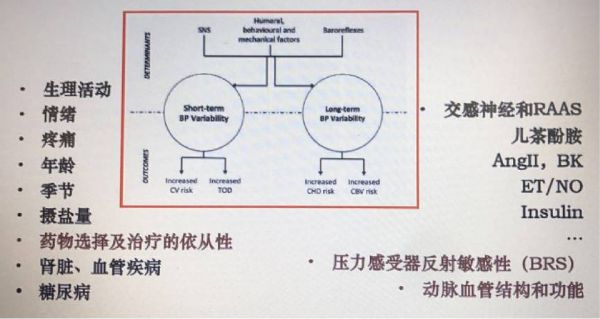
门诊经常有老人来看高血压病,他们往往血压波动大,经常半夜因为血压升高而去急诊降压,希望尽快把血压降下来,其实老年人有特殊的生理特点,降血压也要因人而异。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ACP#
33
#AFP#
47
文章很好.值得分享
71
好文.值得点赞!认真学习.应用于实践!谢谢分享给广大同好!
81
谢谢.学习了
73
#老年高血压#
38
学习了
71
学习
70
谢谢分享.学习了
42
谢谢分享.学习了
34