Dev Cell :利用谱系示踪技术无缝隙捕捉体内肿瘤转移中的EMT过程
2020-07-29 兮 BioArt
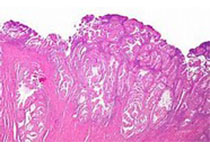
由于乳腺癌细胞丧失了正常的细胞特性,细胞之间的连接变得松散,容易脱落,进入血液系统或者淋巴系统进行转移,在远端器官,如肺,骨,肝等器官处形成转移灶,威胁患者生命。对乳腺癌转移方式及其机理的研究意义重大
乳腺癌是女性群体的最高发癌症,严重威胁着女性患者的生命安全。原发性乳腺癌患者在进行原位肿瘤切除手术治疗后加以适当的放疗或者化疗,具有较好的预后结果。然而由于乳腺癌细胞丧失了正常的细胞特性,细胞之间的连接变得松散,容易脱落,进入血液系统或者淋巴系统进行转移,在远端器官,如肺,骨,肝等器官处形成转移灶,威胁患者生命。因此对于乳腺癌转移方式及其机理的研究意义重大。
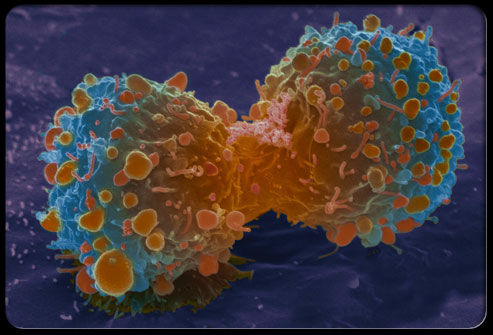
转移的肿瘤细胞是否发生上皮细胞向间充质细胞的转换(epithelial-mesenchymal transition, EMT)一直是肿瘤研究领域的一大热点。并且近几年来对于肿瘤转移过程中的EMT的作用存在争议。EMT过程中,上皮细胞失去其特有的生物学特征,失去细胞极性,失去与基底膜的连接而被赋予一些间充质细胞的特性,细胞形态呈纺锤形,具有比较强的迁移和侵袭能力,具有抗凋亡和降解细胞外基质的能力。前期的研究利用体外细胞培养以及移植的方法认为EMT过程对于肿瘤细胞的转移具有重要的作用,但缺乏直接的体内实验证据,近几年却研究者提出体内肿瘤细胞的转移不需要EMT过程。因此,肿瘤细胞的转移是否发生上皮细胞向间充质细胞的转换有待进一步研究证明。
中国科学院分子细胞科学卓越创新中心周斌研究组在Developmental Cell杂志上在线发表了文章“Genetic Fate Mapping of Transient Cell Fate Reveals N-cadherin Activity and Function in Tumor Metastasis”。该研究成果提示在乳腺癌转移过程中,肿瘤细胞的上皮细胞向间充质细胞转换具有异质性,原位肿瘤细胞会发生N-Cadherin依赖的EMT,并且发生N-Cadherin依赖的EMT的肿瘤细胞贡献形成了大部分的肺转移灶,而原位发生Vimentin依赖的EMT的肿瘤细胞并不会贡献形成肺转移灶,该工作为乳腺癌肿瘤转移的临床防治提供了重要基础信息和新的研究方向。
传统的依赖Cre-LoxP的单同源重组谱系示踪技术虽然可以在体揭示细胞命运,但一般示踪的是他莫昔芬诱导时标记的那群细胞,并且标记的这些细胞的分子标记一般是在细胞中稳定表达的,而诱导型的单同源重组体统难以捕捉体内这些瞬时表达的基因。因此单同源重组系统不适用于示踪肿瘤模型中瞬时的、可逆的EMT过程。在本研究项目中,周斌研究组科研人员基于双同源重组系统创建诱导型的无缝隙谱系示踪技术,以自发性乳腺癌肿瘤模型小鼠MMTV-PyMT为研究对象,利用Kit-CreER来标记小鼠乳腺管腔上皮细胞,构建用于示踪EMT的基因敲入小鼠N-Cad-LSL-Dre和Vim-LSL-Dre,利用双同源报告基因小鼠NR1来同时示踪发生过和未发生过EMT的乳腺肿瘤细胞。
首先研究人员基于前期的双同源重组系统,建立了用于在体捕捉EMT的诱导型无缝隙遗传谱系示踪技术,即EMTracer系统。为研究乳腺肿瘤细胞转移过程中的EMT,研究人员将Kit-CreER;EMTgene-LSL-Dre;NR1( EMTracer小鼠,EMTgene可以是一些公认的间充质细胞的分子标记,例如Vimentin和N-cadherin)与自发性乳腺癌肿瘤模型小鼠MMTV-PyMT配在一起,经他莫昔芬诱导后,Kit-CreER表达的Cre识别报告基因NR1和EMTgene-LSL-Dre两个基因上的LoxP位点发生同源重组。Kit-CreER与报告基因NR1的LoxP发生重组,使Kit+的乳腺管腔上皮细胞被标记上绿色荧光蛋白(ZsGreen),可以谱系示踪Kit+的上皮细胞在乳腺稳态维持中的细胞命运。Kit-CreER与EMTgene-LSL-Dre的LoxP发生重组,使介于两个LoxP之间的stop序列被切掉,当发生上皮细胞向间充质细胞的转换后,EMTgene就会启动表达,使EMTgene后面的Dre表达出来,与报告基因NR1的Rox发生同源重组,使报告基因NR1位于两个Rox位点之间的Rox-LoxP-stop-LoxP-ZsGreen-PolyA-Rox序列被切掉,从而启动红色荧光蛋白(tdTomato)的表达,使发生过EMT的细胞由之前的绿色荧光蛋白(ZsGreen)转变成红色荧光蛋白(tdTomato),实现对EMT的监测。并且,EMTgene-LSL-Dre的stop序列被切掉以后,Dre将持续表达,尽管EMT过程可以是瞬时的、可逆的,利用EMTracer小鼠可以实现对EMT过程的持续监测,弥补了诱导型CreER在监测EMT过程的缺陷,研究人员通过收集肿瘤早期及晚期的原位肿瘤和肺组织进行免疫荧光染色分析肿瘤细胞中的EMT情况,同时通过流式分选将发生过N-Cadherin依赖的EMT的乳腺原位肿瘤细胞分选出来发现这些细胞高表达间充质细胞的分子标记和转录因子。并且这些发生过N-Cadherin依赖的EMT的乳腺原位肿瘤细胞在体外培养具有更强的侵袭能力。
其次,研究人员研究人员还利用N-Cad flox小鼠在乳腺原位肿瘤细胞中特异性敲除N-Cadherin,会减肺转移灶的形成,而Vimentin全敲的乳腺肿瘤小鼠依然可以形成肺转移灶。
该研究结果提示在乳腺癌肿瘤细胞转移的过程中,肿瘤细胞的EMT具有异质性,并且本研究中创建的诱导型无缝隙谱系示踪技术也可以用于发育或者其他肿瘤模型中EMT的研究。
据悉,该研究工作是由博士后李燕,博士生吕赞等在周斌研究员的指导下完成。该研究得到了复旦大学施奇惠教授,暨南大学蔡冬青教授,Albany大学吴明福教授,上海营养健康所胡国宏研究员,香港中文大学吕爱兰教授,南方医科大学冯景教授及西班牙神经研究所Angela Nieto教授的大力协助。
原始出处:
Yan Li, Zan Lv, Shaohua Zhang,et al.Genetic Fate Mapping of Transient Cell Fate Reveals N-Cadherin Activity and Function in Tumor Metastasis.Dev Cell. 2020 Jul 2;S1534-5807(20)30500-1. doi: 10.1016/j.devcel.2020.06.021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dev#
36
#Cell#
28
#CEL#
40
#肿瘤转移#
49
#EMT#
37