Movement disorders:湘雅医院:狗狗嗅一嗅,就能诊断帕金森病?
2022-08-29 Freeman MedSci原创
使用嗅探犬进行测试可能是一种有用的、无创的、快速的和具有成本效益的方法
帕金森病(PD)的诊断可以通过死后的病理检查很好地确定。然而,对于临床医生来说,在许多情况下做出正确的死前诊断仍然是一个巨大的挑战。与病理检查相比,总体准确率为81%。PD诊断的最新标准仍然很复杂,这对非运动障碍专家来说尤其是个问题。
图1: 论文封面图
在许多情况下,对临床上确立的PD进行诊断的时间往往需要数年。需要一种测试来确定PD的诊断,并提高准确性和可重复性。Trivedi及其同事报告说,"超级嗅探者 "可以仅通过气味识别PD,并确定了几种化合物,这些化合物在混合后可以被 "超级嗅探者 "识别为代表PD患者的气味。
长期以来,狗一直被用来搜索非法毒品、爆炸物和失踪人员。最近,越来越多的报告支持狗检测医疗状况的能力,如癌症、疟疾,以及最近的2019年冠状病毒疾病。这些报告表明,嗅探犬可能具有通过嗅觉识别PD的潜力。
因此,湘雅医院的Chang-Qing Gao等人,评估了嗅探犬区分PD患者和非PD对象的能力。
他们在中国的四个三级医疗中心进行了一项前瞻性、诊断性的病例对照研究,评估嗅探犬区分109名临床确定的药物治疗PD患者、654名无PD的受试者、37名药物治疗PD患者和185名非PD对照者的准确性。主要结果是嗅探犬识别的灵敏度和特异度。
他们发现:在对用药患者的研究中,当两只或全部三只嗅探犬在测试的样本中产生阳性检测结果时,指数测试的敏感性、特异性以及阳性和阴性似然比分别为91%(95%CI:84%-96%)、95%(95%CI:93%-97%),以及19.16(95%CI:13.52-27.16)和0.10(95%CI:0.05-0.17)。
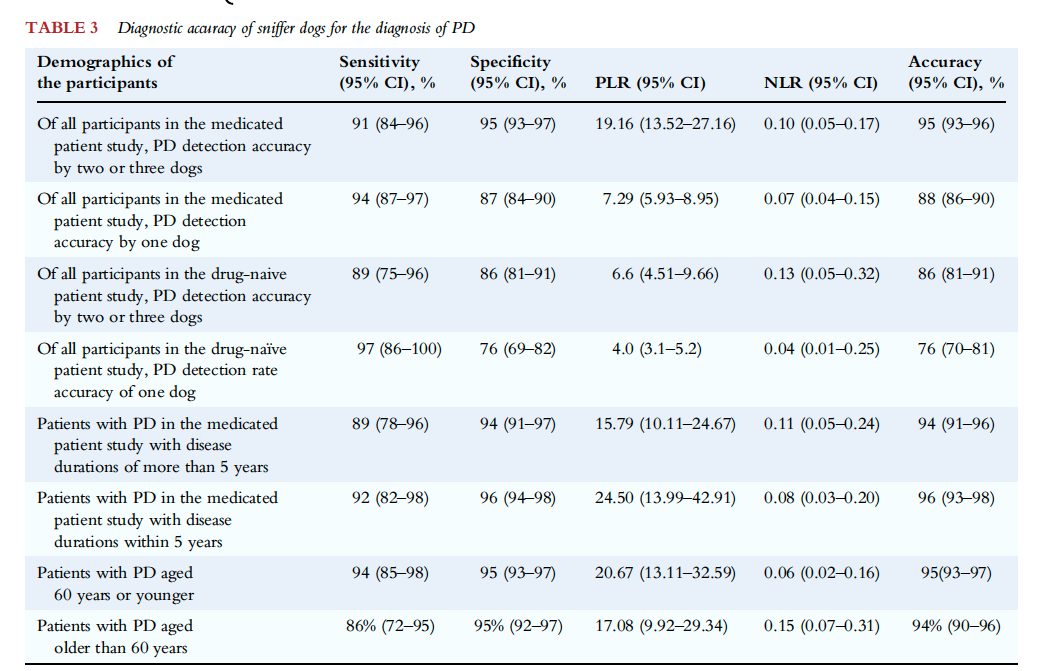 图2:论文结果图
图2:论文结果图
在未用药的患者中,相应的敏感性、特异性、阳性和阴性似然比分别为89%(95%CI:75%-96%)、86%(95%CI:81%-91%),以及6.6(95%CI:4.51-9.66)和0.13(95%CI:0.05-0.32)。
该研究的重要意义在于发现了:使用嗅探犬进行测试可能是一种有用的、无创的、快速的和具有成本效益的方法,可以在社区筛查和健康预防检查以及神经科实践中识别PD患者。
原文出处:
Gao C, Wang S, Wang M, et al. Sensitivity of Sniffer Dogs for a Diagnosis of Parkinson’s Disease: A Diagnostic Accuracy Study. _Movement Disorders_. Published online August 25, 2022:mds.29180. doi:[10.1002/mds.29180](https://doi.org/10.1002/mds.29180)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#ERS#
56
#disorder#
43
#Dis#
58
#Disord#
65
#disorders#
38
#湘雅#
36