Gynecol Oncol&Mol Cancer Ther:阻击卵巢癌生长的阿喀琉斯之踵
2014-06-23 佚名 生物谷
近日,加州大学圣地亚哥分校医学院生殖医学系教授David D. Schlaepfer博士带领下的一组科学团队报告:小分子抑制剂抑制粘着斑激酶(FAK)能选择性预防卵巢癌细胞的生长。 这项发现发表在Gynecologic Oncology和Molecular Cancer Therapeutics杂志上。卵巢癌是女性癌症死亡的首要原因。平均而言,每年美国,超过21,000名妇女诊断患有卵巢癌,1
近日,加州大学圣地亚哥分校医学院生殖医学系教授David D. Schlaepfer博士带领下的一组科学团队报告:小分子抑制剂抑制粘着斑激酶(FAK)能选择性预防卵巢癌细胞的生长。
这项发现发表在Gynecologic Oncology和Molecular Cancer Therapeutics杂志上。卵巢癌是女性癌症死亡的首要原因。平均而言,每年美国,超过21,000名妇女诊断患有卵巢癌,14,270名患者死亡。许多妇女疾病会缓解,但癌症的复发率超过75%,这就提示需要新的治疗方法。
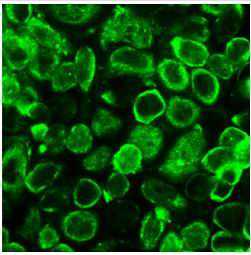
卵巢癌细胞通过一个独特的机制,即通过涉及小簇肿瘤细胞(称为球体)的生存在妇女腹膜间隙内的扩散,Schlaepfer说:我们的研究表明,FAK信号功能在肿瘤细胞存活信号网络中发挥中心作用。
第一项研究发表在Gynecologic Oncology杂志上,第一作者Nina Shah医师等发现低水平肿瘤抑制蛋白merlin的卵巢肿瘤细胞,显示对FAK抑制剂高度的敏感性,研究结果支持这一假设:蛋白质生物标志物如merlin可以识别哪些患者可能是最好响应FAK抑制剂疗法。
第二项研究发表在Molecular Cancer Therapeutics,第一作者Isabelle Tancioni博士发现骨桥蛋白生成的信号网络(骨桥蛋白是β-5整合素受体)在细胞与细胞之间的信号传导中发挥作用;FAK控制卵巢癌球体的增长,高水平的β-5整合素和FAK表达与一些卵巢癌患者预后差相关联。因此,高水平的β-5整合素可作为一种新的生物标志物,用于指示具有活化FAK信号的卵巢癌细胞。
Schlaepfer指出,肿瘤的复发和转移是导致大多数卵巢癌有关死亡的原因,新的研究结果支持了在进行中的临床试验,即粘着斑激酶抑制剂是防止卵巢癌进展的新药物。
原始出处:
Shah NR1, Tancioni I1, Ward KK1, Lawson C1, Chen XL1, Jean C1, Sulzmaier FJ1, Uryu S1, Miller NL1, Connolly DC2, Schlaepfer DD3.Analyses of merlin/NF2 connection to FAK inhibitor responsiveness in serous ovarian cancer.Gynecol Oncol. 2014 Jul;134(1):104-111. doi: 10.1016/j.ygyno.2014.04.044. Epub 2014 Apr 27.
Tancioni I1, Uryu S2, Sulzmaier FJ1, Shah NR1, Lawson C1, Miller NL3, Jean C1, Chen XL4, Ward KK1, Schlaepfer DD5.FAK inhibition disrupts a beta5 integrin signaling axis controlling anchorage-independent ovarian carcinoma growth.Mol Cancer Ther. 2014 Jun 4. pii: molcanther.1063.2014. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
30
很好,有帮助
128
#NEC#
30