JAMA neurology:尼洛替尼对中晚期帕金森患者的疗效
2021-01-02 MedSci原创 MedSci原创
尼洛替尼具有可接受的安全性和耐受性,但低CSF暴露和缺乏生物标志物效应,加上疗效数据呈负面趋势,提示尼洛替尼不应该在PD中进一步测试。
帕金森病(PD)是第二大常见的神经退行性疾病,影响了1%的65岁以上的人口。PD症状通常随时间缓慢出现,早期最明显的症状为颤抖、肢体僵硬、运动功能减退和步态异常,晚期会发生认知和行为问题。此外,痴呆症在病情严重的PD患者中相当常见,超过三分之一的病例也会发生重性抑郁障碍和焦虑症。

虽然药物的开发日益进步,但目前的药物仍未满足减缓PD进展的需求。
尼洛替尼(Nilotinib)可以抑制BCR-Abl而被获批用于慢性粒细胞白血病的治疗。但近年来的动物研究却发现,尼洛替尼在PD动物模型中具有神经保护作用。这一发现激起了人们开发尼洛替尼以减缓PD进展的兴趣。
然而,尼洛替尼的安全性和耐受性仍未知。此前,尼洛替尼在PD治疗中的临床经验仅来自于一项小型的研究。随后,2020年报道了同一小组开展的一项2期临床试验结果,表明尼洛替尼在中度晚期PD中表现出可接受的安全性和耐受性,并对PD生物标志物起了改善作用,但对临床结果没有显著影响。
为此,美国西北大学与NILO-PD国际研究组的专家团队进行了一项多中心RCT研究,旨在评估尼洛替尼在参与者中的安全性和耐受性。
该研究是一项为期6个月、多中心、随机平行组、双盲、安慰剂对照的试验。患者招募时间为2017年11月20日至2018年12月28日,随访于2019年9月9日结束。该研究在美国25个临床中心进行。研究最初筛选了173名患者,其中48名患者拒绝,125名患者接受研究。最终,76名接受PD药物治疗方案的患者入组。
参与者以1:1:1随机接受安慰剂、150 mg尼洛替尼或300 mg尼洛替尼治疗,每日一次口服,持续6个月,随后进行2个月的非药物评价。
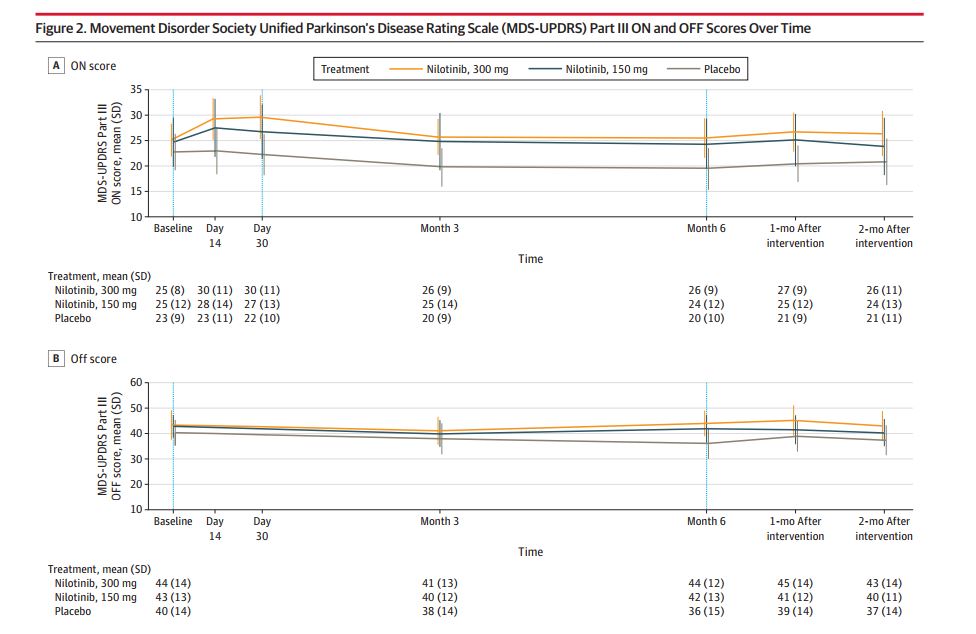
主要结果是药物的安全性和耐受性。次要结果包括PD残疾的变化(MDS-UPDRS评分第二部分OFF/ON)。探索性结果包括血清和CSF药代动力学特征,以及CSF多巴胺能生物标志物。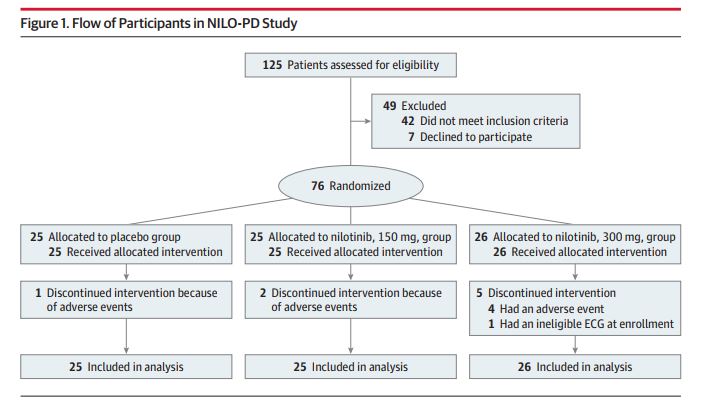
参与者的平均基线年龄为64.6岁,平均病程为9.9年。MDS-UPDRS第1-3部分OFF评分为66.4分,ON评分为48.4分,蒙特利尔认知评估(MOCA)评分为27.1分。在安慰剂、150 mg和300 mg臂中,接受指定剂量的参与者完成研究的人数分别为21人(84%)、19人(76%)和20人(77%),两种活性剂量的安全性均可接受。
其中最常见的停药原因是无症状的、剂量依赖性的淀粉酶、和/或脂肪酶的升高。在第1个月时,与安慰剂相比,尼洛替尼150 mg和300 mg都表现出更差的MDS-UPDRS-3 ON评分。但从基线到6个月,组间MDS-UPDRS-3 OFF的变化没有差异。脑脊液/血清比尼洛替尼浓度为0.2%~0.3%。没有证据表明CSF中多巴胺代谢物的治疗相关改变。
基于上述研究结果,研究人员认为,尼洛替尼具有可接受的安全性和耐受性,但低CSF暴露和缺乏生物标志物效应,加上疗效数据呈负面趋势,提示尼洛替尼不应该在PD中进一步测试。
参考文献:
Simuni T, et al. Efficacy of Nilotinib in Patients With Moderately Advanced Parkinson Disease: A Randomized Clinical Trial. JAMA Neurol. 2020 Dec 14:e204725. doi: 10.1001/jamaneurol.2020.4725.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
34
#尼洛替尼#
37
谢谢梅斯提供这么好的信息,学到很多
45
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
59