Cell Reports:西湖大学新发现:尿液中的蛋白可作为新冠轻重型的分类标准
2022-01-07 “生物世界”公众号 “生物世界”公众号
过去两年来,新冠的爆发让全人类措手不及。截至今天,新冠病毒仍然在地球上大部分地区肆虐。凛冬已至,温度骤降,现在已经进入了感冒等流行病毒的高发季节。
过去两年来,新冠的爆发让全人类措手不及。截至今天,新冠病毒仍然在地球上大部分地区肆虐。凛冬已至,温度骤降,现在已经进入了感冒等流行病毒的高发季节。随着新的突变株奥密克戎(Omicron)的出现,世界上已经有不少国家对此警戒万分,全球人类也需要共同协作,以控制新一轮新冠的爆发。不管是哪一变株流行,其背后的基础研究都是迫切和必要的。尿液分子表型的研究有重大意义。
近日,西湖大学西湖实验室郭天南课题组等在 Cell Reports 发表了题为:Proteomic and metabolomic profiling of urine uncovers immune responses in patients with COVID-19 的研究论文。

该研究表明新冠肺炎病人的尿液作为一种完全无创的生物样本,从尿液中获取的生物分子可以灵敏地反映机体的病理状态。这项研究从尿液中筛选出 20 个蛋白质标志物并建立模型,成功实现了对新冠患者进行分类预测的目的;该研究同时针对性地提出了新冠患者存在潜在肾损伤的证据。
尿液来源于外周循环,无需专业采集手段即可获得(相比较血清、组织等),完全可以满足日常实时健康监测的要求。利用尿液中的生物分子对人体健康状态进行监测,对于未来精准医学、精准抗疫具有重要的实用价值和现实意义。
该研究对 COVID-19 患者组以及健康对照组的共计 115 个尿液、血清样本进行了系统研究。运用蛋白组学和代谢组学的分析手段,对各组病人进行了研究对比。从蛋白层面分析,单位体积的尿液蛋白表达量在轻、重型 COVID-19 组中与健康组相比明显升高,这个结果提示尿液可能会更灵敏地反应机体疾病水平的变化。
该研究共定量了 1494 个血清蛋白,3854 个尿液蛋白,903 个血清代谢物和 1033 个尿液代谢物。研究发现尿液中的蛋白分子量分布与全人类蛋白组的蛋白分子量分布一致,这说明尿液样本不会漏掉某一类蛋白而导致信息丢失。
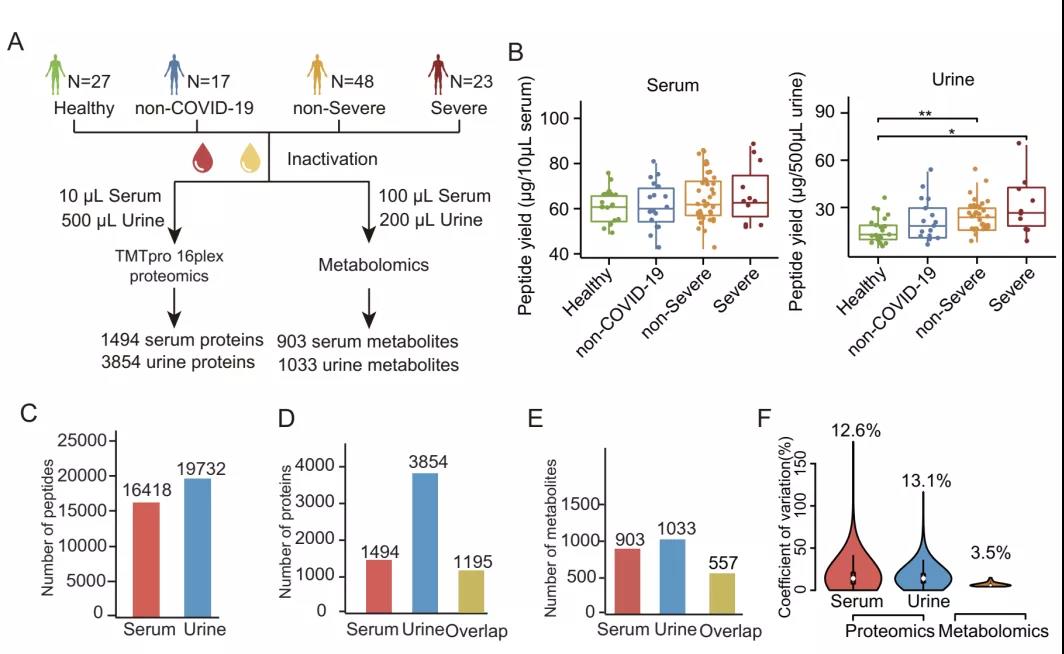
血清和尿液蛋白质组学和代谢组学数据汇总分析
那么尿液蛋白能否体现出新冠肺炎引起的分子变化呢?机器学习结果显示,尿液蛋白对于轻重型新冠肺炎的区分能力与血清蛋白基本一致。该研究在此基础上,建立了基于 20 个尿液蛋白的机器学习模型。在重型 COVID-19 患者的转归过程中,该模型的预测值随着时间的延长逐渐降低;而在轻型的恢复患者中,预测值趋于平缓并无明显变化。这些结果进一步证实了这 20 个尿液蛋白具备对 COVID-19 轻重型进行分类预测的潜力。
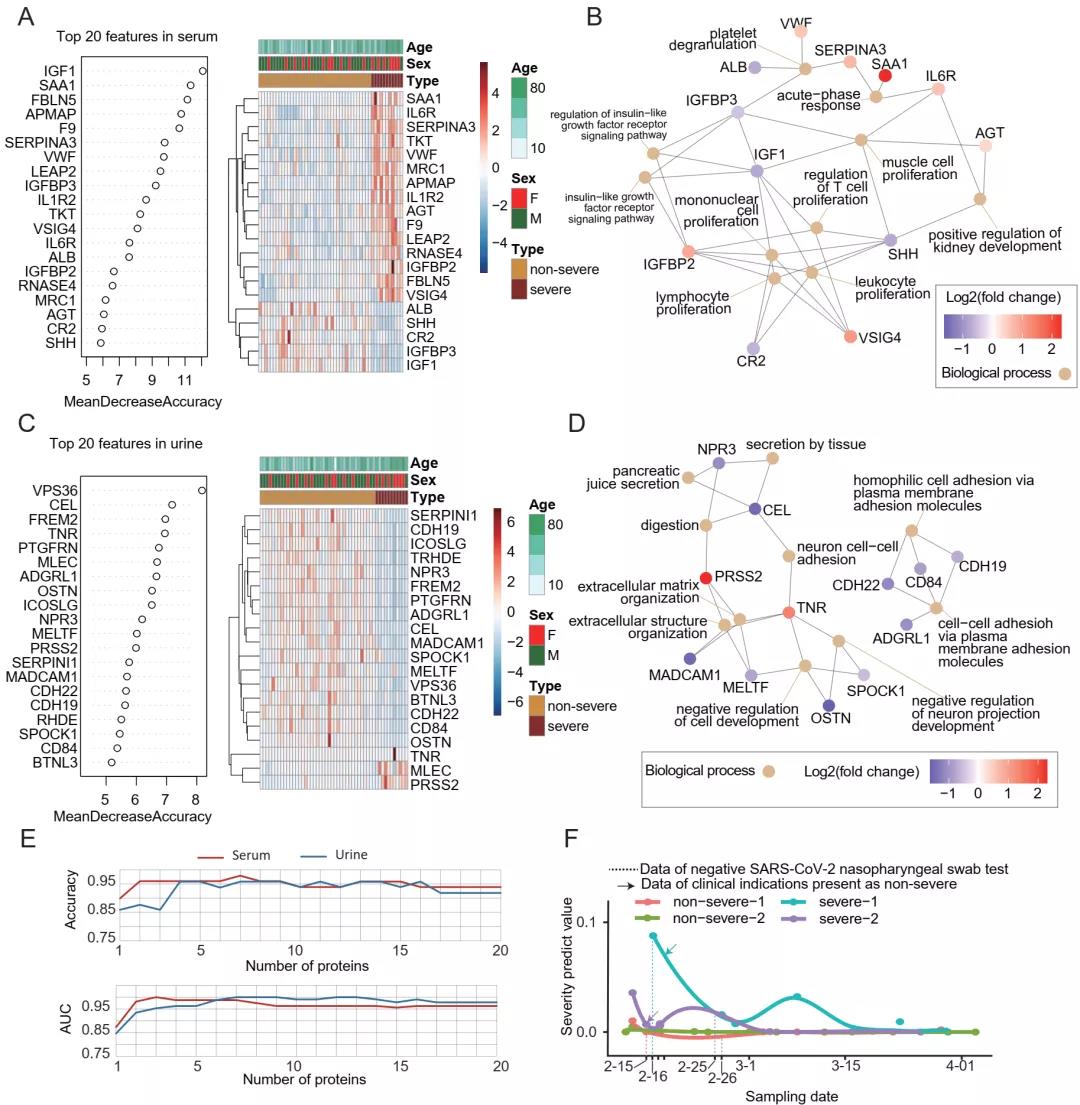
在蛋白质组学水平上区分轻型和重型 COVID-19 患者
该研究接下来探索了 COVID-19 患者血清和尿液之间的相关性。随着疾病进程加重(健康-轻型-重型),有 301 个蛋白的相对丰度在尿液和血清中呈现出相反的表达模式。
研究发现两种参与肾小管重吸收的重要调节因子,megalin (LRP2) 和 cubilin (CUBN),在 COVID-19 患者尿液中的含量均呈现下降趋势。COVID-19 患者的肾小管再吸收过程可能出现了紊乱失调,导致尿液中某些蛋白质变化呈现出与血液中不同的表达模式。这种现象可能也存在于其他疾病中,还有待进一步研究。
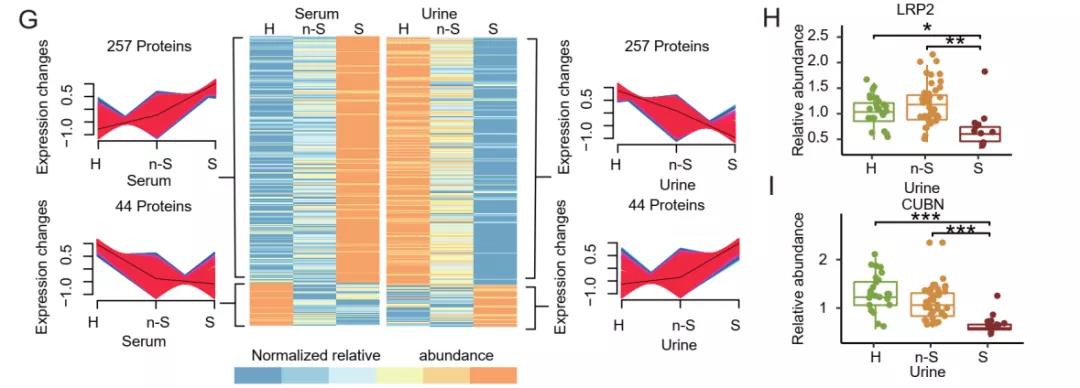
301 个血清和尿液蛋白显示出相反的表达模式
不受控制的先天性炎症反应引起的细胞因子风暴,是导致 COVID-19 患者高死亡率的主要原因,因此该研究还着重关注了细胞因子在血清和尿液中的表达情况。该研究在血清中定量到了 124 个细胞因子,在尿液中定量到了 197 个。在尿液中,CXCL14 与 COVID-19 患者的淋巴细胞计数具有显着的相关性,或可能用于指示 COVID-19 病情的严重程度。
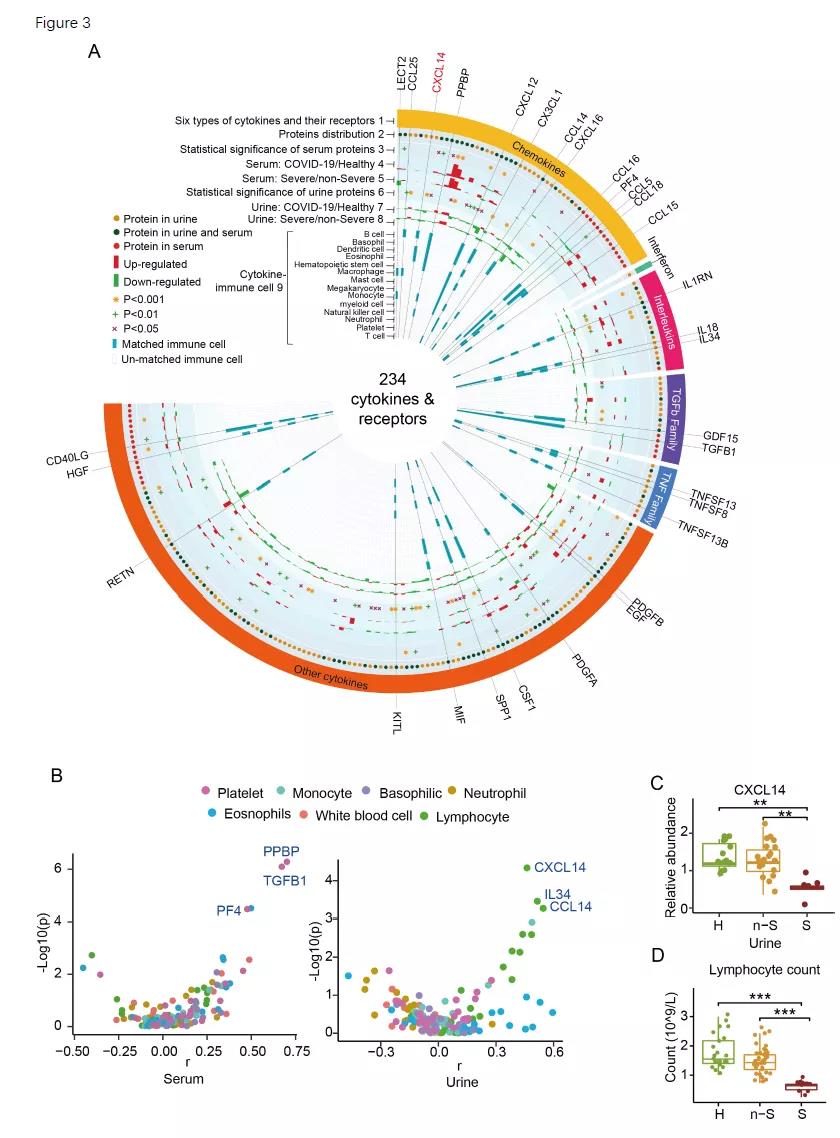
尿液和血清中的细胞因子特征
此外,该研究还在尿液蛋白组中特异性地发现了一些与病毒出芽相关的蛋白,它们在 COVDI-19 患者的尿液中呈现显着的下调趋势,且未在血清中检测到。以上结果表明在这一研究里,尿液蛋白组显示了比血液蛋白组更高的检测灵敏度。
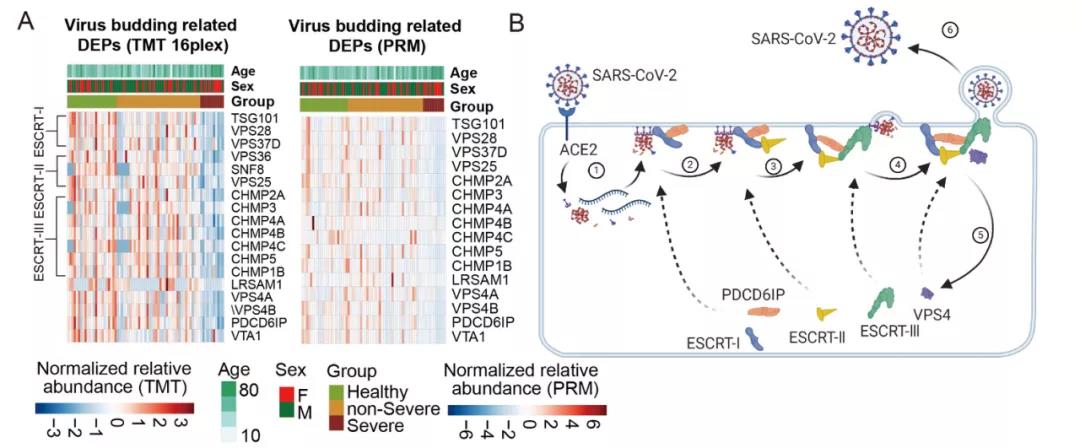
尿液中定量到的与病毒出芽相关的蛋白在健康对照和 COVID-19 患者中呈现差异表达模式
该研究通过差异通路分析,得到了许多在差异表达通路中频繁出现的蛋白。其中 Rho GTP 酶家族的 CDC42、RAC1/RAC2 和 RHOA 出现的频率最为频繁。这些蛋白的失调可能会导致肾小球硬化和肾脏损伤。此外,肾脏足细胞-肌动蛋白的动态调节需要消耗大量ATP。代谢组学数据显示,腺苷(ATP 代谢的产物)含量在重型 COVID-19 患者的尿液中明显降低,这进一步表明患者体内可能存在足细胞运动障碍和潜在的肾脏损。

COVID-19 患者血清和尿液中失调蛋白质分析
像其他病毒感染一样,SARS-COV-2 会通过打破体内氧化和抗氧化系统之间的平衡而引发氧化应激反应。从该研究的代谢组学数据中可以发现,多种抗氧化因子如牛磺酸、次牛磺酸和1-甲基烟酰胺 (1-MNA) 在 COVID-19 患者的血清中显着下调。在蛋白层面,该研究也发现 SOD3 和 GPX4 等多种抗氧化酶在重型 COVID-19 的尿液中显着下调。这一切都显示新冠患者体内可能存在 ROS 激活的应激反应。
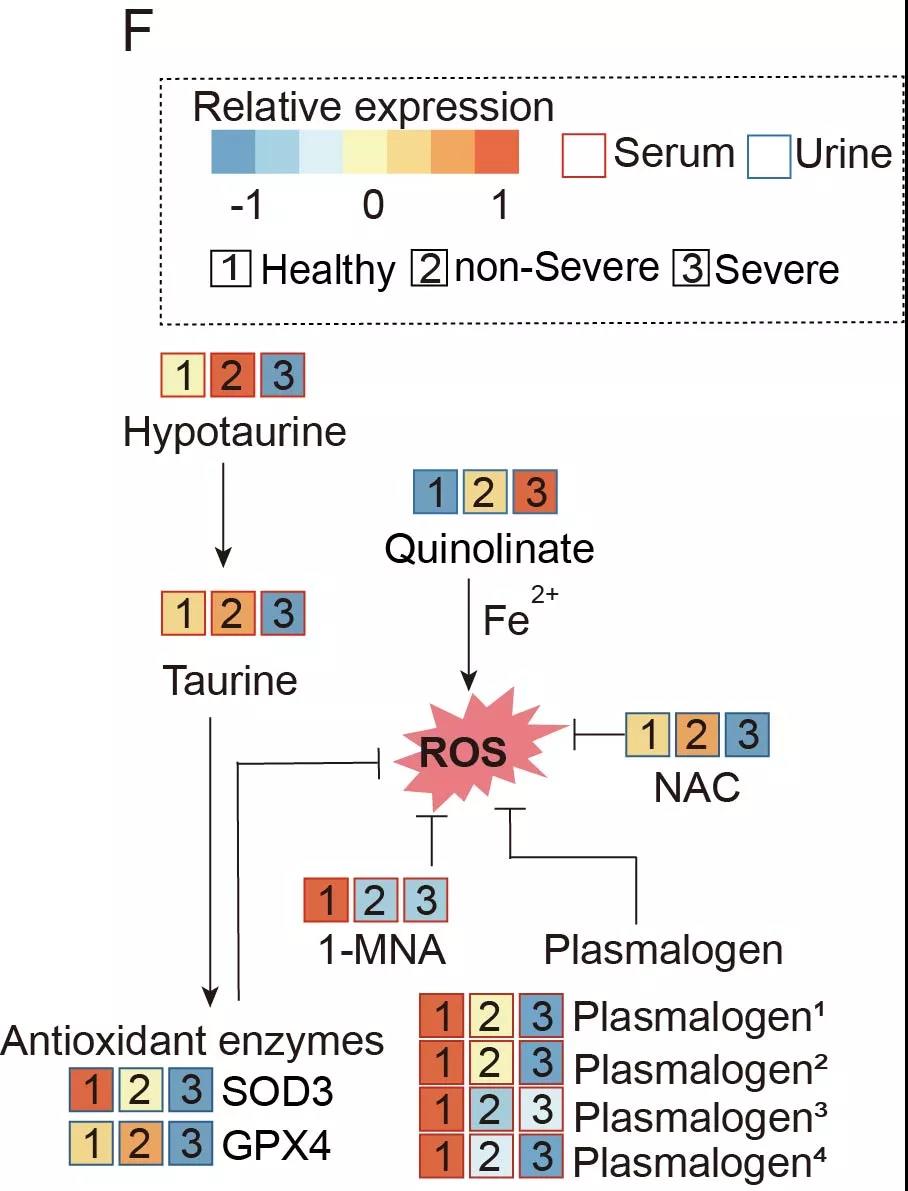
COVID-19 患者血清和尿液中失调的代谢物分析
基于以上线索,该研究全面解读新冠肺炎患者尿液及血液的多组学数据中异常改变的分子和信号通路,并推测出患者体内新冠病毒引起的分子通路水平的改变和调节机制:免疫紊乱触发的炎症反应、凝血反应以及细胞纤维化会最终损伤肾组织。临床数据也显示,重型患者的各型肾损伤指标虽然仍在正常范围内,但是相对于健康对照组,已经发生了显着的改变。上述结果都表明 SARS-COV-2 可能造成肾损伤。该研究最终提出,要密切关注新冠患者肾损伤的临床指征,并在新冠康复后保持对肾脏功能的跟踪观察。
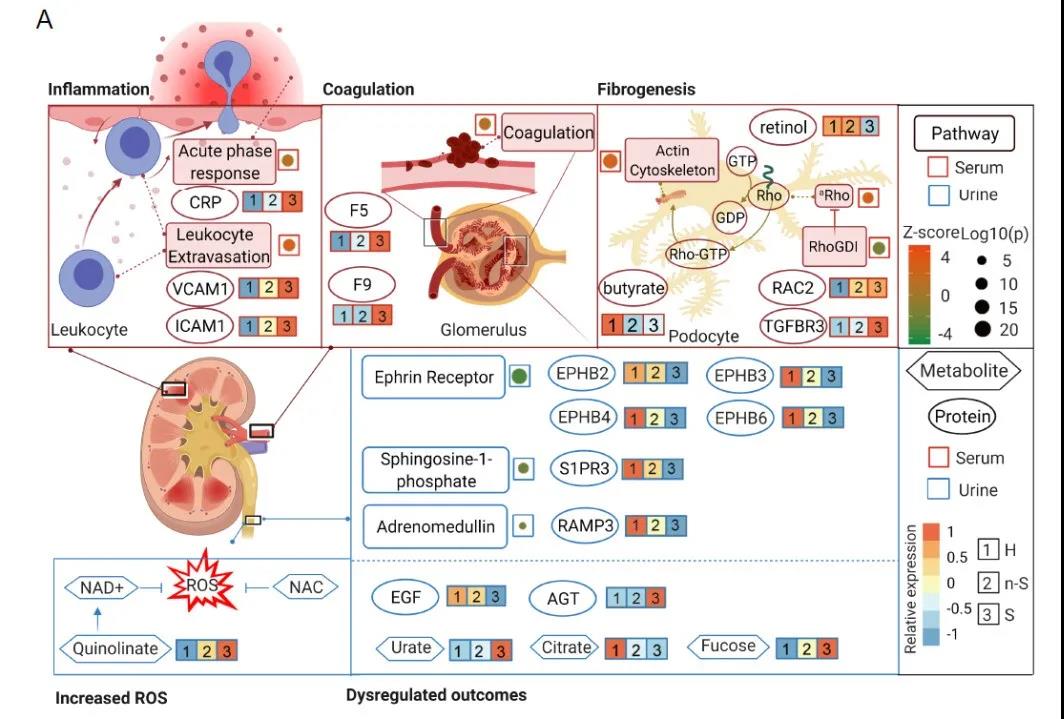
重型 COVID-19 患者免疫失调和 ROS 激活诱导肾损伤的模型

郭天南课题组合影
郭天南课题组主要从事高通量蛋白质组学和临床大数据研究,使用独特的循环压力技术(Pressure Cycling Technology) 高通量的处理超小量的临床样本, 借助高通量的 SWATH 卫星扫描质谱技术将其蛋白组数字化,开发机器学习算法分析蛋白质组大数据,探索在各种生理和病理状态下蛋白质表达和变化的数学规律,致力于实现基于蛋白质组的精准医疗。
原始出处:
Xiaojie Bi, et al. Proteomic and metabolomic profiling of urine uncovers immune responses in patients with COVID-19. Cell Reports, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CEL#
28
#新发现#
34
#Cell#
29
#分类标准#
33
#尿液#
53
不错学习了。
46