JAMA Oncol:3期随机试验:序贯放化疗 vs 同步放化疗用作早期宫颈癌术后辅助治疗的疗效
2021-01-15 Nebula MedSci原创
本研究旨在评估序贯放化疗(SCRT)和同步放化疗(CCRT)与单纯放疗(RT)相比作为早期宫颈癌术后辅助治疗的临床疗效。
对于有不良病理因素的早期宫颈癌患者,除了放疗外,化疗作为术后辅助治疗的作用尚未达成共识。本研究旨在评估序贯放化疗(SCRT)和同步放化疗(CCRT)与单纯放疗(RT)相比作为早期宫颈癌术后辅助治疗的临床疗效。
本研究是一项在中国8家医院中开展的3期随机试验,招募根治性子宫切除术后的、有不良病理因素的IB~IIA期宫颈癌患者。随机分为3组,分别接受辅助RT、CCRT或SCRT。主要终点是3年无病生存率(DFS)。
2008年2月-2018年12月,共招募了1048名患者(中位年龄48[23-65]岁):RT组350人,CCRT组345人,SCRT组353人。除了RT组淋巴结受累率最低(18.3%)外,各治疗组的基线人口学和疾病特征均衡。
预后
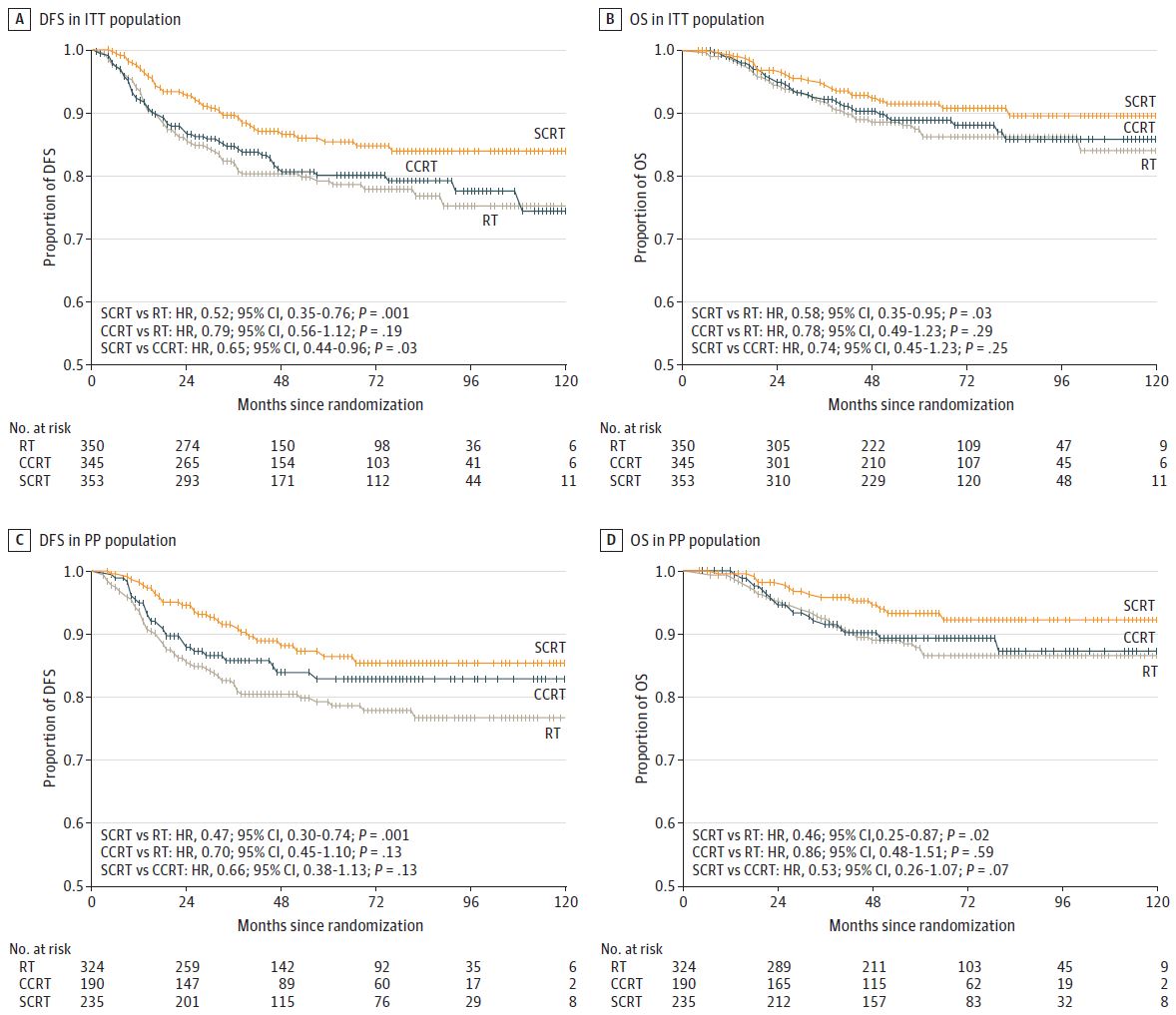
在意向治疗人群中,与RT相比,SCRT与更高的DFS率相关(3年DFS率:90.0% vs 82.0%;危险比[HR]0.52,95%CI 0.35-0.76);与CCRT相比,SCRT仍与更高的DFS率相关(90.0% vs 85.0%;0.65,0.44-0.96)。与RT相比,SCRT治疗还可降低癌症死亡风险(5年生存率:92.0% vs 88.0%;HR 0.58,95%CI 0.35-0.95)。然而,在接受CCRT或RT治疗的患者中,DFS和癌症死亡风险都没有差别。
综上,该研究显示,对于早期宫颈癌患者,相比CCRT,SCRT治疗能更好的提高DFS率和降低癌症死亡风险。
原始出处:
Huang He,Feng Yan-Ling,Wan Ting et al. Effectiveness of Sequential Chemoradiation vs Concurrent Chemoradiation or Radiation Alone in Adjuvant Treatment After Hysterectomy for Cervical Cancer: The STARS Phase 3 Randomized Clinical Trial. JAMA Oncol, 2021. https://doi.org/10.1001/jamaoncol.2020.7168
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
.JPG)












#术后辅助治疗#
52
#Oncol#
40
#放化疗#
44
#宫颈#
36
#随机试验#
31
#同步放化疗#
33
谢谢梅斯提供这么好的信息,学到很多
55
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
47
谢谢梅斯分享这么多精彩信息
48
高质量研究,读起来真爽,谢谢梅斯
55