European Radiology:CCTA的左房功能是心衰和心血管死亡的预测因子
2022-02-16 shaosai MedSci原创
尽管最近心脏病的治疗效果有所改善,但心力衰竭(HF)仍然是一种预后极差的常见疾病。越来越多的证据表明,左心房(LA)重构和功能障碍可能作为疾病进展的调节因素和症状发展的预测因素而发挥重要作用。
尽管最近心脏病的治疗效果有所改善,但心力衰竭(HF)仍然是一种预后极差的常见疾病。越来越多的证据表明,左心房(LA)重构和功能障碍可能作为疾病进展的调节因素和症状发展的预测因素而发挥重要作用。
心脏计算机断层扫描血管造影(CCTA)是一项真正的等轴三维技术,可提供快速、自动的基于体素的LA体积计算。这项技术可为评估LA重塑和功能提供更好的敏感性和准确性,可以更好地岁高HF风险患者进行早期识别。然而据我们所知,关于从CCTA评估的LA相位容积和功能的相关研究十分稀少。
近日,发表在European Radiology杂志的一项研究在一大群连续接受CCTA的患者中,评估了LA功能的容积指数与HF相关的临床结果之间的关系,为高危患者的早期识别及干预提供了可能。
在788名连续接受螺旋CT扫描的正常窦性心律患者中,使用自动推导LA体积来计算LA总排空分数(LATEF)以评估LA功能。使用Cox模型分析了CCTA评估的LATEF与因HF入院或CV死亡的复合终点之间的关系。
在4年的中位随访期间,共发生了100起事件,62例HF住院,38例心血管疾病死亡。有事件和无事件的患者的平均LATEF分别为30.7±10.7%和40.5±11.2%(P<0.0001)。高LATEF(上三分位数>46%)与极低的事件发生率有关(6年时为3.5%[95% CI 1.7-7.1%])。相对于最高的三分位数,最低的LATEF三分位数的HF或CV死亡率的调整HR为4.37(95% CI 1.99-9.60),中间三分位数为2.29(95% CI 1.03-5.14)。对于单纯的HF终点,LATEF最低三分位数的调整后HR为5.93(95% CI 2.23-15.82),中间三分位数为2.89(95% CI 1.06-7.86)。对于左心室射血分数降低和保留的患者,LATEF与结果的关系相似(Pinteraction = 0.724)。即使在LA容积正常的情况下,LATEF降低也与高事件发生率有关。
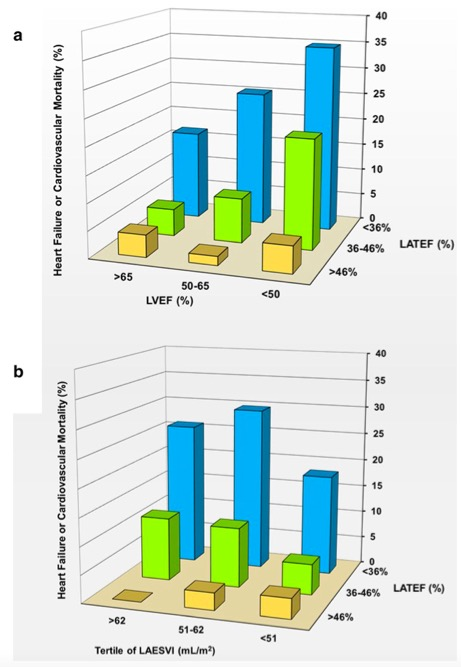
a LATEF和LVEF的分位数与心力衰竭和心血管死亡率的关系。 b LATEF的分位数和左心房收缩末期容积指数的分位数与心力衰竭和心血管死亡率的关系。
本研究表明,LATEF与未来的HF入院和CV死亡密切相关,与临床危险因素及LV大小和功能无关。即使LA容积正常,LATEF降低也预示着HF和心血管疾病死亡的发生。LATEF可以成为CCTA分析的一个重要组成部分,并在所有覆盖整个心脏周期的动态扫描中进行报告。
原文出处:
Jonathan Lessick,Diab Mutlak,Michael Mutlak,et al.Left atrial function by cardiac computed tomography is a predictor of heart failure and cardiovascular death.DOI:10.1007/s00330-021-08093-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CCT#
38
#PE#
29
#CTA#
34
#预测因子#
54
#心血管死亡#
49