PLOS MED:300万人数据提示,孕期焦虑、失眠使用苯并二氮䓬类药物增加后代畸形的风险
2022-03-23 网络 网络
孕期头三个月的苯二氮卓暴露与整体畸形和心脏缺陷的风险增加有关,特别是在较高的日剂量下。
焦虑、失眠和情绪障碍在怀孕期间很常见,苯二氮卓类药物经常被开给孕妇来处理这些情况。世界范围内孕期使用苯二氮卓类药物的流行率约为2%,而在韩国,超过1%的孕妇在怀孕前三个月被开具这些药物。
尽管苯并二氮䓬类药物经常被使用,但在过去的几十年里,随着人们对新型抗抑郁药或抗精神病药的关注度不断提高,苯并二氮䓬类药物使用安全性的证据仍缺乏。然而,关于可能的致畸性的证据并不明确。

为了评估孕期头三个月使用苯二氮卓类药物与主要先天性畸形风险之间的关系,来自韩国的学者利用韩国的全国性医疗数据库对2011-2018年期间分娩的妇女及其活产婴儿进行了基于人口的队列研究。结果发表在PLOS MEDICINE杂志上。
暴露被定义为在怀孕的前三个月有一个或多个苯二氮卓类药物的处方。确定了总体先天性畸形和12种特定器官畸形的相对风险(RRs)和置信区间(CIs)。对婴儿从出生到死亡或2019年12月31日(以先到者为准)进行随访(至8岁)。
在总共3094227名孕妇中,有40846人(1.3%)在怀孕前三个月暴露于苯二氮卓类药物(平均[SD]年龄,32.4 [4.1]岁)。暴露于苯并二氮䓬类药物的孕妇中,总体畸形的绝对风险为65.3/1000,而未暴露的孕妇为51.4/1000。调整后风险升高9%(RR=1.09,95%CI 1.05-1.13,P<0.001),总体畸形升高15%(1.10-1.21,P<0.001)。
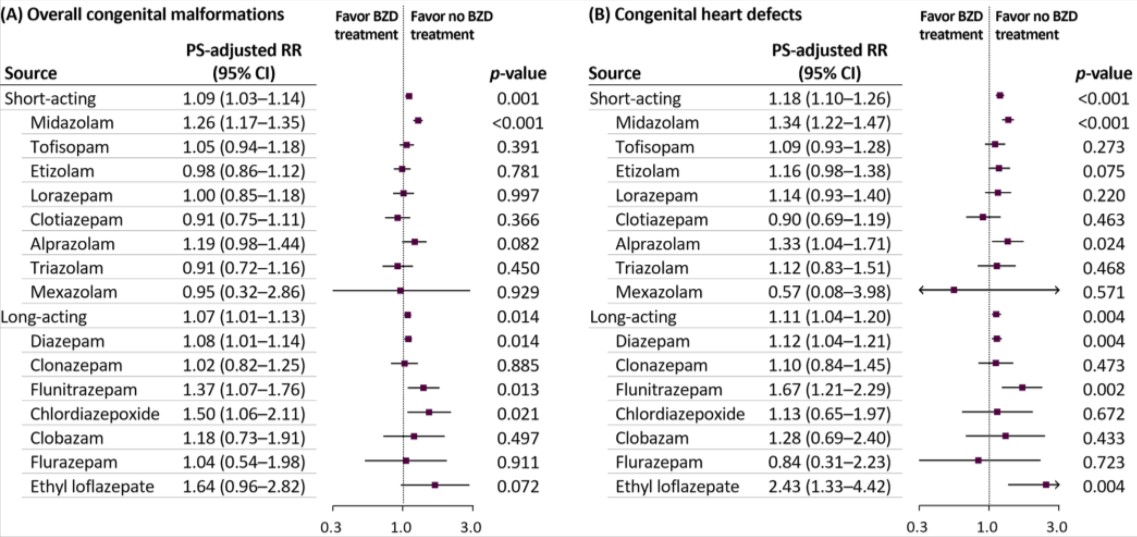
基于每日劳拉西泮的平均剂量,调整后的总体畸形和心脏缺陷风险升高5%(0.99-1.12,P = 0.077)和12%(1.04-1.21,P = 0. 004),>2.5毫克/天的剂量则分别为26%(1.17-1.36,p<0.001)和31%(1.19-1.45,p<0.001),表明有剂量反应关系。
综上,孕期头三个月的苯二氮卓暴露与整体畸形和心脏缺陷的风险增加有关,特别是在较高的日剂量下。
参考文献:
First-trimester exposure to benzodiazepines and risk of congenital malformations in offspring: A population-based cohort study in South Korea. https://doi.org/10.1371/journal.pmed.1003945
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
56
#畸形#
43
#Med#
27