Magn Reson Med:组织的T1信号在动脉自旋标记测量脑血流量时的影响
2016-05-09 MedSci MedSci原创
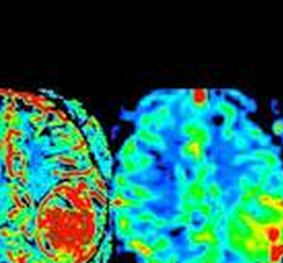
研究目的:动脉自旋标记可以提供定量的脑血流量的地形图。因为标记的水和结合水相交换,这项研究评估了组织T1信号在使用动脉自旋标记定量测量脑血流量时的影响。研究方法:为了对T1信号进行修饰,低剂量的锰在19只老鼠的一侧半球中脑内注射(在皮质或者纹状体),组织T1信号和脑血流量通过在4.7T磁共振上使用翻转复原及联系的动脉自旋标记序列获得地形图。研究结果:当通过动态磁敏感和弥散加权成像评估时,发现锰减少
研究目的:动脉自旋标记可以提供定量的脑血流量的地形图。因为标记的水和结合水相交换,这项研究评估了组织T1信号在使用动脉自旋标记定量测量脑血流量时的影响。
研究方法:为了对T1信号进行修饰,低剂量的锰在19只老鼠的一侧半球中脑内注射(在皮质或者纹状体),组织T1信号和脑血流量通过在4.7T磁共振上使用翻转复原及联系的动脉自旋标记序列获得地形图。
研究结果:当通过动态磁敏感和弥散加权成像评估时,发现锰减少了组织的T1信号超过30%,但是对别的组织特性很少有影响。使用单室模型,发现单一的组织T1值在锰注射侧比非注射侧皮层减少34%,纹状体减少22%。使用T1地形图,其数值各自变为-7% 和 +8%。
研究结论:低剂量的锰减少组织T1值而不改变脑血流量。不同的T1对动脉自旋标记评估脑血流量在独立区域有影响。在动物上,当T1改变超过组织T1被定义的精度是,当使用动脉自旋标记测量脑血流量是应该获得组织T1的评估。
原始出处:
Debacker CS1,2,3, Daoust A1,2, Köhler S3, Voiron J3, Warnking JM1,2, Barbier EL1,2.et al,Impact of tissue T1 on perfusion measurement with arterial spin labeling.,Magn Reson Med. 2016 May 2. doi: 10.1002/mrm.26255. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脑血流#
36
#血流量#
58
#动脉自旋标记#
43
#ESO#
45
#Med#
45
学习了,希望有新的突破!
126