Nat Comm: 抑制肠道中树突状细胞的CD40通路治疗肠炎
2017-03-16 Leo.c MedSci原创
CD40通路的激活破坏了CD103+树突状细胞促使抑制炎症的Treg细胞的产生。针对CD40通路进行干预可以促使Treg细胞产生,从而抑制过激的肠道免疫反应及肠炎。
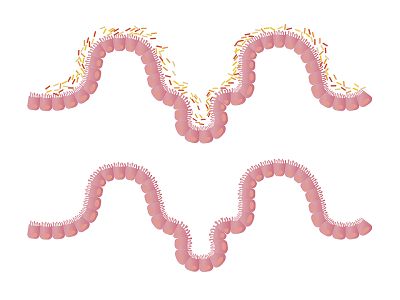
人的肠道系统存在数以万计的共生菌。为了不使这些共生菌引起过强的免疫反应,在肠道中有大量的Treg 细胞来维持共生菌和免疫系统的平衡。肠道中的巨噬细胞(macrophages)以及树突状细胞(dendritic cells)起到识别共生菌然后在引流淋巴结(draining lymph node)中帮助产生大量的Treg 细胞来抑制免疫系统对这些共生菌的免疫反应。然而,肠道中的树突状细胞同时也产生促炎因子包括IL-17A和IFN-γ。机体是如何平衡肠道中的树突状细胞进行抑制或促进免疫反应的功能?
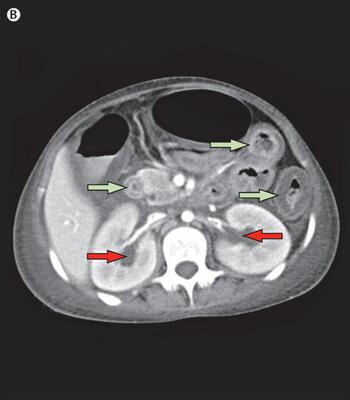
在本期的Nature Communication杂志中,Christian Barthels 及其同事证明了CD40/CD40L信号通路的激活对肠道中的树突状细胞的功能起到重要作用。本文的作者们通过使用基因编辑后的老鼠,使实验鼠的树突状细胞持续激活CD40通路,发现肠道中的CD103+树突状细胞从肠道黏膜(lamina propia)移动到肠系膜淋巴结(mesenteric lymph node),从而在肠道黏膜有减少数量的树突状细胞以及Treg 细胞。也因此导致了肠道中的促炎的Th1/Th17细胞的免疫反应增强导致肠道细菌紊乱以及严重的肠炎。
这项研究揭示,CD40通路的激活破坏了CD103+树突状细胞促使抑制炎症的Treg细胞的产生。针对CD40通路进行干预可以促使Treg细胞产生,从而抑制过激的肠道免疫反应及肠炎。
原始出处:
Christian Barthels, Ana Ogrinc, Verena Steyer, et al., CD40-signalling abrogates induction of RORγt+ Treg cells by intestinal CD103+ DCs and causes fatal colitis. Nature Communications 8, Article number: 14715 (2017) doi:10.1038/ncomms14715
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CD4#
33
#Nat#
29
感谢分享,学习了
50
谢谢分享,好好学习
0