Gut:选择性COX-2抑制剂塞来昔布单用对胃癌癌前病变有效
2011-10-15 MedSci原创 MedSci原创
由香港大学、北京大学肿瘤医院及山东省临朐县卫生局相关研究人员共同开展的一项最新研究显示,环氧合酶-2(COX-2)抑制剂塞来昔布治疗或单纯幽门螺杆菌(Hp)根除治疗有益于晚期胃部病变(Advanced Gastric Lesions)的逆转,而Hp根除治疗后的塞来昔布治疗并没有获得良好效果。该研究于9月13日在线发表于《消化》(Gut)杂志。 Hp感染和COX-2的过度表达与胃癌及癌前相
由香港大学、北京大学肿瘤医院及山东省临朐县卫生局相关研究人员共同开展的一项最新研究显示,环氧合酶-2(COX-2)抑制剂塞来昔布治疗或单纯幽门螺杆菌(Hp)根除治疗有益于晚期胃部病变(Advanced Gastric Lesions)的逆转,而Hp根除治疗后的塞来昔布治疗并没有获得良好效果。该研究于9月13日在线发表于《消化》(Gut)杂志。
Hp感染和COX-2的过度表达与胃癌及癌前相关。为评估选择性COX-2抑制剂单用及其与Hp根除治疗联用对癌前胃部病变进展的影响,研究人员Benjamin C Y Wong等在山东省临朐县开展了一项随机、安慰剂对照试验。他们随机将1024名Hp感染和晚期胃部病变的患者(年龄35~64岁)分至干预组或安慰剂组:抗Hp感染治疗7天;COX-2抑制剂塞来昔布治疗24个月。通过晚期胃部病变的逆转或进展来评估干预效果(详见下表)。
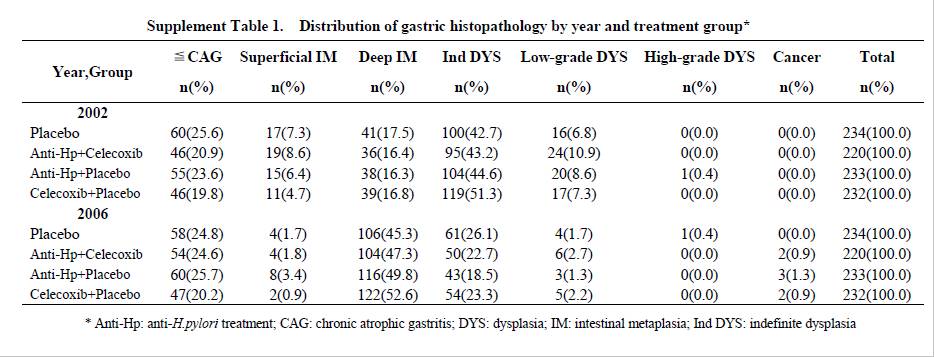
结果:共有1024名受试者接受了抗Hp治疗或安慰剂,919名完成了随后的24个月塞来昔布治疗或安慰剂;经过分析,Hp根除率为78.2%;塞来昔布治疗和抗Hp治疗组胃部病变的逆转比率较安慰剂组显著增加,分别为52.8%对41.2%,59.3% 对41.2%,比值比分别为1.72(塞来昔布)和2.19(Hp根除);Hp根除治疗后的塞来昔布治疗对晚期胃部病变的逆转未发现有显著影响(OR 1.48)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抑制剂#
30
#2抑制剂#
36
#选择性#
41
#COX-2抑制剂#
42
#塞来昔布#
30
#COX-2#
41