先天性心脏病相关肺动脉高压患者缺损修复围手术期血浆代谢组学研究
2021-12-03 刘少飞 MedSci原创
通过缺损修复手术和个性化治疗,先天性心脏病相关肺动脉高压(CHD-PAH)患者的生活质量和生存率得到了极大改善。然而,手术后存活的患者仍可能面临持续性 PAH 的风险,预后可能比未手术的患者差得多。
与先天性心脏病 (CHD) 相关的肺动脉高压 (PAH) (CHD-PAH) 是 PAH 最常见的病因之一,其特征是由房间隔缺损、室间隔缺损、小动脉导管未闭和动脉导管未闭引起的分流病变。其他分流型先天性心脏病。大约 5%–10% 的青少年和成年 CHD 患者会发展为PAH。CHD-PAH患者通常与特发性和其他相关形式的PAH患者有一些相似之处,尤其是在非特异性的主要症状方面。CHD-PAH患者可能会遇到社会限制以及因疾病负担而引起的情绪和心理问题。CHD-PAH的发展可导致终生损害。然而,CHD–PAH的预后优于特发性PAH,因为其死亡风险是单纯CHD患者的两倍以上。CHD-PAH是发展中国家最常见的肺血管疾病亚型,约占43%,是欧美发达国家发病率的3-4倍。
随着对肺血管疾病认识的深入,代谢异常被确定为CHD-PAH发生发展的重要病理基础。在肺血管狭窄、闭塞和右心衰竭的过程中,组织和血液中的代谢特征发生了强烈的变化。由于分流矫正比常规药物治疗效果更迅速,CHD-PAH患者肺循环代谢物的变化可能更直观地反映肺血管的阻塞和流动。代谢物的变化也将为疾病逆转的反应提供重要信息。例如,先前的研究表明,可以监测内皮素水平,以识别法洛四联症伴发绀的患者,其对体外循环 (CPB) 表现出增强的炎症反应的风险增加。紫绀型CHD婴儿中较高的缺氧/高氧介导的S100B水平更容易出现围手术期脑应激/损伤。此外,与闭合心脏手术相比,CHD新生儿的血清血影蛋白分解产物在心脏直视手术后增加的程度更大,表明血清血影蛋白分解产物可能作为患有冠心病的婴儿脑坏死和细胞凋亡的生物标志物。然而,尚无研究试图系统地解读 CHD-PAH 患者围手术期缺损修复期间血液代谢物的动态特征。因此,在CHD-PAH患者缺损修复手术围手术期的不同时间点进行了血浆代谢组学研究,并检查了代谢改变是否通过治愈性手术得到纠正。与此同时,我们试图找出表明临床管理中对分流矫正反应更好的临床措施。
临床队列:
2013年7月至2016年7月,中国医学科学院阜外医院连续招募13例CHD-PAH患者,采集其血样用于缺损修复手术围手术期的代谢组学研究。CHD-PAH 的诊断基于 2015 年 ESC/ERS 肺动脉高压诊断和治疗指南的标准。排除标准为:年龄<18岁或>60岁,主要并发症包括高血压、高血脂、乙肝、糖尿病,或肿瘤或代谢性疾病家族史。该研究遵循赫尔辛基宣言中关于人类医学研究的伦理原则。研究方案经中国医学科学院阜外医院伦理委员会批准,并获得每位受试者的书面知情同意书。
样本采集和临床措施
CHD-PAH患者在围手术期进行缺损修复手术时,在以下时间点从上腔静脉采集3 mL血样,置于预冷的EDTA抗凝管中:麻醉后体外循环(CPB)前( Pre)、CPB 后立即 (T0)、手术后 24 h (T24) 和 48 h (T48)。采血后,将血样在 4 °C 下以 4000 r/min 的速度离心10分钟。将分离的血浆样品放入液氮中并转移至-80 °C,然后再使用。样品处理前无反复冻融,避免代谢物潜在降解风险。在围手术期的四个不同时间点记录临床指标,包括来自所有 CHD-PAH 患者的心率 (HR)、血流动力学和血气分析以及来自所有 CHD-PAH 患者的肺动脉和桡动脉(临床指标)在 T48 时仅在 12 名 CHD-PAH 患者中可用)。
液相色谱-质谱分析
在维持在45 °C的 ZORBAX Eclipse Plus C18色谱柱上对处理过的血浆样品进行液相色谱分离,而在Nexera X2 系统与三重 TOF 5600 四极杆飞行时间质谱仪相结合。样品室的温度保持在7°C。在全定量环进样模式下,每次运行进样量为 10 μL,流动相流速为 0.5 mL/min。流动相 A 主要由水组成,含有 0.1% 的甲酸。流动相 B 主要由乙腈组成,含有 0.1% 的甲酸。水(LC-MS 级)和乙腈(LC-MS 级)购自 Fisher Scientific。Acros 的甲酸纯度大于 98%。
研究结果:
在这项研究中,我们探讨了13名CHD-PAH患者在缺损修复围手术期的血浆代谢物谱。在四个时间点采集血浆:麻醉后体外循环 (CPB) 前 (Pre)、体外循环 (CPB) 后立即 (T0)、缺损修复后 24 小时 (T24) 和 48 小时 (T48)。基于UPLC Q-TOF MS 的非靶向代谢组学策略用于检测代谢物。在不同时间点共测定了 193 种不同的代谢物,富含支链脂肪酸氧化等途径。
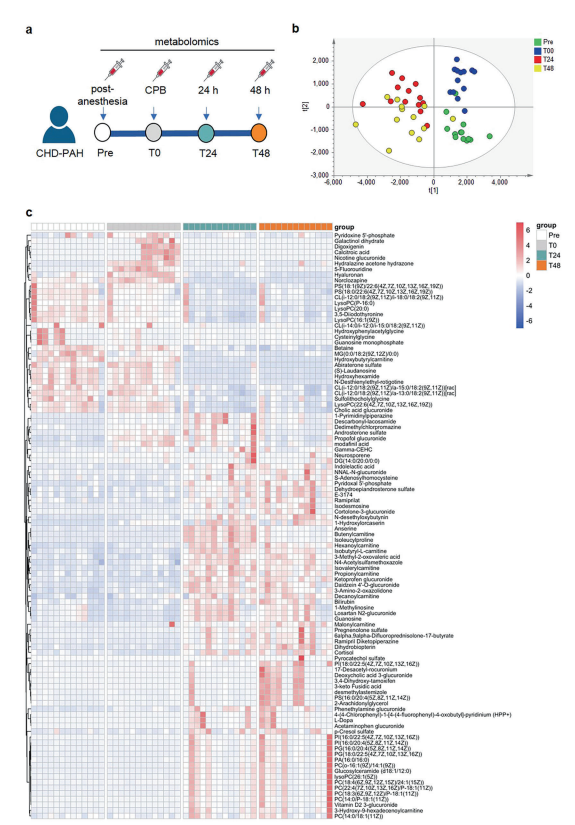
13名CHD-PAH 患者围手术期代谢谱的总体比较分析(上图)
我们发现 17 种代谢物的改变与 T48 与 Pre 的平均肺动脉压 (MPAP) 的降低显着相关。舒张期肺动脉压 (DPAP)、桡动脉碳酸氢盐 (aHCO) 的梯度3 )、上腔静脉碳酸氢盐(svcHCO 3 )、桡动脉溶解CO 2气体分压(aPCO 2 )) 与 MPAP 梯度呈正相关。值得注意的是,这些临床测量梯度与分流矫正相关代谢物的改变相关。
总的来说,在 T24 和 T48 时,17 种鉴定出的对缺陷修复有反应的代谢物中有 12 种增加(所有 P < 0.05,除了丙酰肉碱在 T24 时 P < 0.05)。相比之下,半乳糖醇二水合物、鸟苷一磷酸和羟基苯乙酰甘氨酸在 T24 和 T48 趋于下降(仅半乳糖醇二水合物在 T48 时 P < 0.05)。总之,对分流矫正有反应的 17 种代谢物可用作合适的无创标志物和临床指标,包括 DPAP、aHCO 3、svcHCO 3和 aPCO 2,将在疾病监测和评估未来的治疗干预方面具有重要价值。
参考文献:
He YY, Yan Y, Chen JW, Liu S, Hua L, Jiang X, Xu XQ, Lu D, Jing ZC, Yan FX, Han ZY. Plasma metabolomics in the perioperative period of defect repair in patients with pulmonary arterial hypertension associated with congenital heart disease. Acta Pharmacol Sin. 2021 Nov 30. doi: 10.1038/s41401-021-00804-3. Epub ahead of print. PMID: 34848852.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肺动脉高压患者#
44
#组学研究#
43
#手术期#
41
#动脉高压#
42
#先天性#
40
#代谢组#
55