NEJM:PDE4B抑制剂BI 1015550 可防止特发性肺纤维化患者肺功能下降
2022-06-14 zhangfan MedSci原创
PDE4B抑制剂BI1015550单独使用或联合抗纤维化药物可有效防止特发性肺纤维化患者肺功能下降,且安全性良好。
特发性肺纤维化(IPF)是一种进行性、不可逆的肺部疾病,患者死亡率很高。目前,已有两种药物——Nintedanib和Pirfenidone上市,其可以减缓但不能阻止纤维化进展。磷酸二酯酶4(PDE4)抑制与抗炎和抗纤维化相关,其中PDE4B亚型抑制可能对IPF治疗有益。近日研究人员公布了PDE4B抑制剂BI 1015550 II期临床的研究结果。
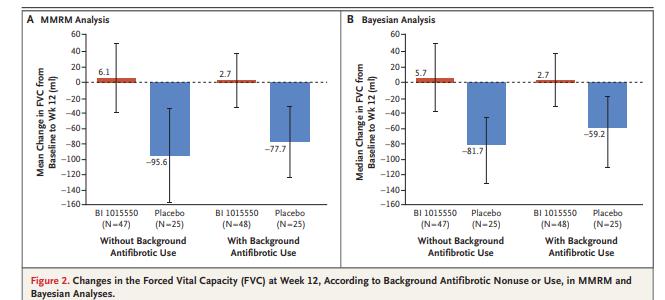
本次II期双盲、安慰剂对照试验中,研究人员考察了BI 1015550对特发性肺纤维化患者的疗效和安全性。患者随机接受BI 1015550,剂量为18 mg,每日两次或安慰剂。研究的主要终点是12周时用力肺活量(FVC)较基线的变化。
共有147名患者参与研究。在没有使用抗纤维化药物的患者中,BI 1015550组FVC的平均变化为5.7 ml,安慰剂组为-81.7 ml(平均差异88.4 ml)。在使用抗纤维化药物的患者中,BI 1015550组FVC的平均变化为2.7 ml,安慰剂组为-59.2 ml(平均差异62.4 ml)。BI 1015550组最常见的不良事件是腹泻,共有13名患者因不良事件停止治疗。组间严重不良事件率相似。
研究认为,PDE4B抑制剂BI1015550单独使用或联合抗纤维化药物可有效防止特发性肺纤维化患者肺功能下降,且安全性良好。
原始出处:
Luca Richeldi et al. Trial of a Preferential Phosphodiesterase 4B Inhibitor for Idiopathic Pulmonary Fibrosis. N Engl J Med,June 9, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#特发性#
50
#肺功能下降#
0
#抑制剂#
41
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
56
NEJM上果然牛,感谢梅斯更新及时
48