Circ Res: PPIs可加速血管内皮细胞的老化
2016-05-13 MedSci MedSci原创
Circ Res: PPIs可加速血管内皮细胞的老化近日来自休斯敦卫理公会研究院的一项新的研究揭示了质子泵抑制剂诱导身体健康问题的机制,该研究已发表于Circulation Research。质子泵抑制剂(PPI)是治疗胃食管反流的常用药物,目前供患者长期使用而并没有医疗监督。最近的研究结果表明,PPI的使用与心血管、肾脏和神经系统疾病的发生有关。该研究探究了PPIs对患者血管内皮功能障碍和老化的
质子泵抑制剂(PPI)是治疗胃食管反流的常用药物,目前供患者长期使用而并没有医疗监督。最近的研究结果表明,PPI的使用与心血管、肾脏和神经系统疾病的发生有关。
该研究探究了PPIs对患者血管内皮功能障碍和老化的长期影响,并探究PPI诱导血管功能障碍的机制。
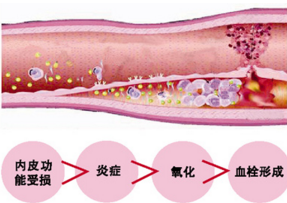
研究人员解释,健康人的血管内皮细胞可产生一个聚四氟乙烯样的涂层,可防止血液粘附,但是当内皮细胞老化或发生疾病时,血管内皮细胞变得更像魔术贴一样,血液成分很容易附着在上面形成血栓。
该结果发现长期暴露于PPIs可损害血管内皮功能,并可缩短端粒的长度从而加速人类内皮细胞的衰老。
PPIs与胃质子泵的结合不可逆转,几乎可完全阻止胃酸的分泌。但是,在这个过程中PPIs似乎还可影响溶酶体。
溶酶体广泛存在机体细胞中,利用酸来清理和分解细胞垃圾。该研究结果发现,PPIs阻止溶酶体产生充足的酸。换句话说,PPIs削弱了溶酶体清理细胞垃圾的能力,导致细胞过早老化。而另一种药物H2 antagonists则不会产生这样的作用。
研究人员希望该研究结果有助于说服官方机构为PPIs的使用制定更加严格的指导方针。
除非另有说明,医生应该只考虑PPIs短期使用,因为该研究结果明确表明PPIs长期使用的危害。
某些情况下或可通过改变生活方式,使用H2受体拮抗剂或手术来控制胃食管反流病。
目前的研究仅限于体外研究,因此需要在人类的研究以证实本研究结果。如果体内研究结果也是如此,那么最终将会改变目前PPIs的使用。
Tim Newman.Heartburn drug
prematurely ages blood vessels. MNT, 11 May 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血管内皮细胞#
55
以后好好利用一下
106
真心的好
116
希望能够有更好的东西
187
很不错啊
154
怎么这么好的东西都么人
49
我觉得真的好
139
真心不错
140
真心不错
62
#PPIs#
54