冠状动脉造影是诊断冠状动脉粥样硬化性心脏病(冠心病)的一种常用而且有效的方法,是一种较为安全可靠的有创诊断技术,现已广泛应用于临床,被认为是诊断冠心病的“金标准”。冠脉造影只能显示直径大于0.5mm血管。
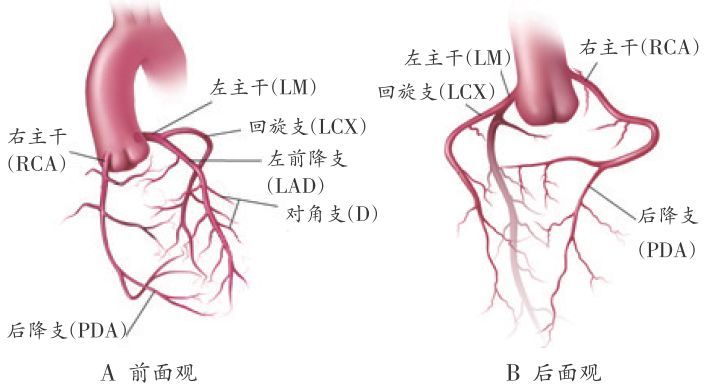
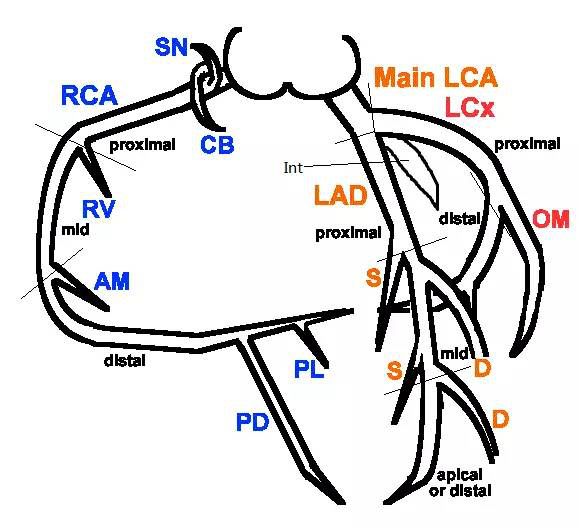
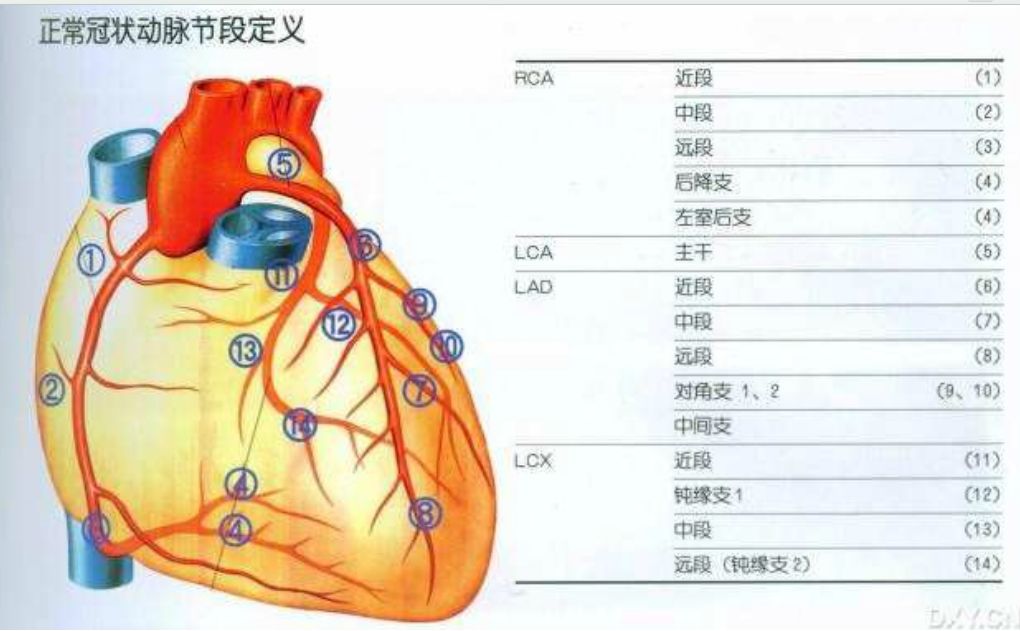
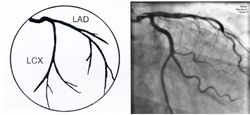
冠状动脉解剖及命名
冠状动脉走行于心脏表面,环绕心脏分布,主要有两大分支:左冠状动脉和右冠状动脉。
➤左冠状动脉主干(LM)起源于升主动脉左后方的左冠窦,行至前室间沟时分为左前降支(LAD)和左回旋支(LCX)。
---前降支通常供应部分左室、右室前壁及室间隔前2/3的血液,其分支分别向三个方向发出,即对角支(D)、右室前支、室间隔支。
---左回旋支主要供应左心房壁、左心室外侧壁、左心室前后壁的一部分;主要分支有钝缘支(OM)。
➤右冠状动脉(RCA)开口于升主动脉右前方的右冠窦,供应右心房、右心室前壁与心脏膈面的大部分心肌;主要分支有后降支(PD)、左室后支(PL)等。
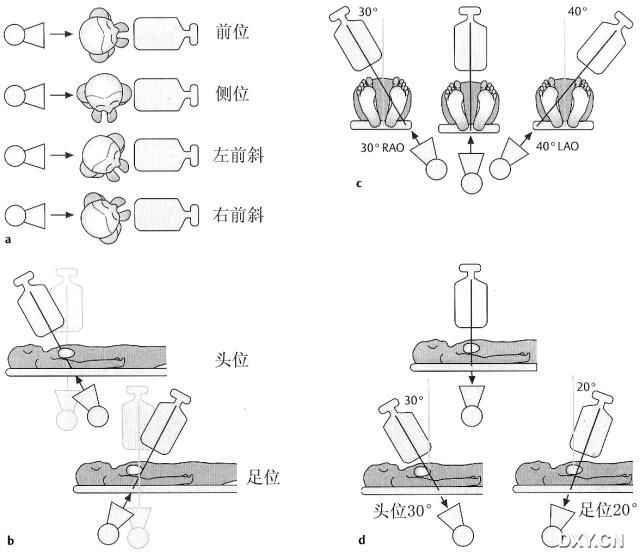
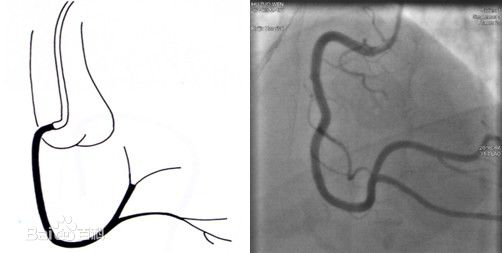
左冠状动脉造影常用的投照体位可以简便记忆为:观测方向绕心脏顺时针旋转一圈(如:头-左肩-左腰-足-右腰-右肩)
正头位:正位+头位------AP+CRA
左肩位:左前斜+头位---LAO+CRA
蜘蛛位:左前斜+足位---LAO+CAU
正足位:正位+足位------AP+CAU
肝位:右前斜+足位---RAO+CAU
右肩位:右前斜+头位---RAO+CRA
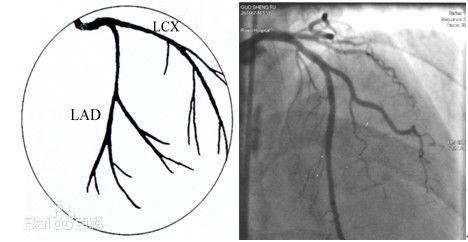
正头位:正位+头位:观察LAD近、中段,LAD与对角支分叉处
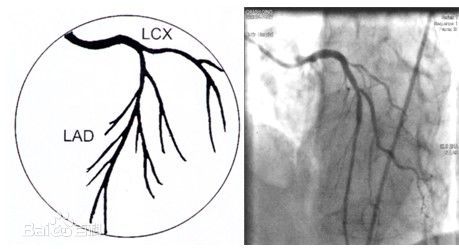
左肩位:左前斜+头位:观察LAD中、远段和对角支开口
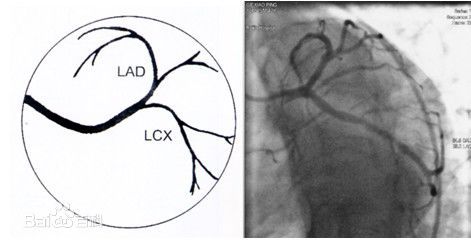
蜘蛛位:观察LM、LAD、LCX开口病变,LCX体部、OM开口和体部
肝位:右前斜+足位:观察LAD、LCX起始部、LCX体部、OM 开口和体部
右冠状动脉造影常用的投照体位:(左侧倾斜或头位)
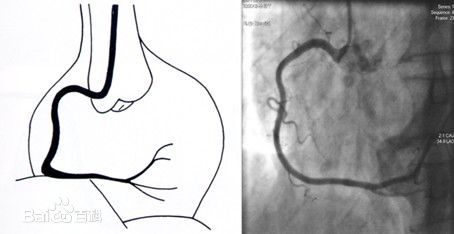
左前斜:RCA呈“C”型,观察RCA开口、起始部至后降支
后前位+头位:RCA呈“L”型,观察RCA远端分支及其开口情况
冠状动脉造影的适应证
以诊断为主要目的
1.不明原因的胸痛或心律失常,需冠状动脉造影除外冠心病。
2.不明原因的左心功能不全,主要见于扩张型心肌病或缺血性心肌病,两者鉴别往往需要行冠状动脉造影。
3.经皮冠状动脉介入治疗(PCI)或冠状动脉旁路移植术后复发心绞痛。
4.先天性心脏病和瓣膜病等重大手术前,年龄>50岁,其易合并有冠状动脉畸形或动脉粥样硬化,可以在手术的同时进行干预。
5.无症状但疑有冠心病,在高危职业如:飞行员、汽车司机、警察、运动员及消防队员等或医疗保险需要。
以治疗为主要目的
临床冠心病诊断明确,行冠状动脉造影可进一步明确冠状动脉病变的范围、程度,选择治疗方案。
⒈稳定型心绞痛或陈旧心肌梗死,内科治疗效果不佳,影响学习、工作及生活。
⒉不稳定型心绞痛,首先采取内科积极强化治疗,一旦病情稳定,积极行冠状动脉造影;内科药物治疗无效,一般需紧急造影。对于高危的不稳定型心绞痛患者,以自发性为主,伴有明显心电图的ST段改变及梗死后心绞痛,也可直接行冠状动脉造影。
⒊发作6小时以内的急性心肌梗死(AMI)或发病在6小时以上仍有持续性胸痛,拟行急诊PCI手术;如无条件开展PCI术,对于AMI后溶栓有禁忌的患者,应尽量转入有条件的医院。AMI后静脉溶栓未再通的患者,应适时争取补救性PCI。对于AMI无并发症的患者,应考虑梗死后1周左右择期行冠状动脉造影。AMI伴有心源性休克、室间隔穿孔等并发症应尽早在辅助循环的帮助下行血管再灌注治疗。对于高度怀疑AMI而不能确诊,特别是伴有左束支传导阻滞、肺栓塞、主动脉夹层、心包炎的患者,可直接行冠状动脉造影明确诊断。
⒋无症状性冠心病,其中对运动试验阳性、伴有明显的危险因素的患者,应行冠状动脉造影。
⒌CT等影像学检查发现或高度怀疑冠状动脉中度以上狭窄或存在不稳定斑块。
⒍原发性心脏骤停复苏成功、左主干病变或前降支近段病变的可能性较大的均属高危人群,应早期进行血管病变干预治疗,需要评价冠状动脉。
⒎冠状动脉旁路移植术后或PCI术后,心绞痛复发,往往需要再行冠状动脉病变评价。
冠状动脉造影的禁忌证
⒈对碘或造影剂过敏。
⒉有严重的心肺功能不全,不能耐受手术者。
⒊未控制的严重心律失常如室性心律失常。
⒋电解质紊乱。
⒌严重的肝、肾功能不全者。
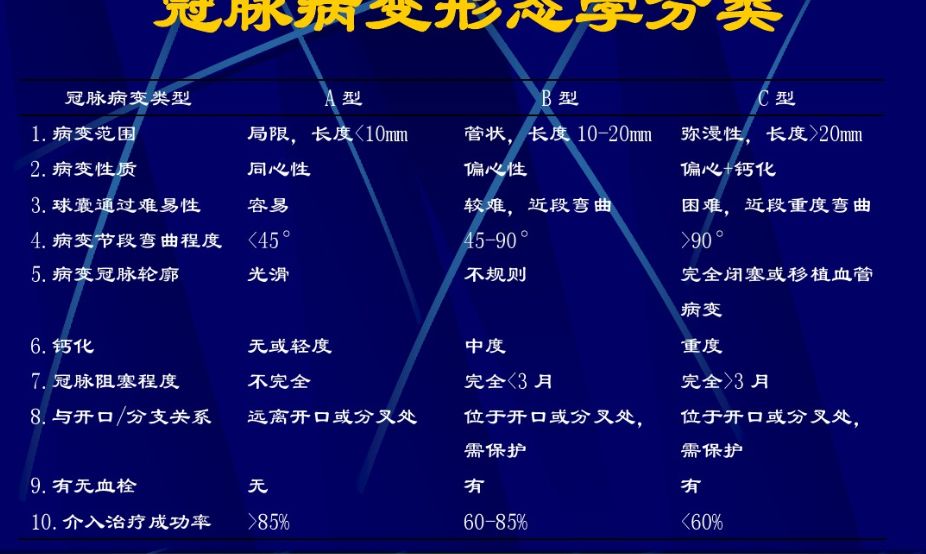
Proudilit冠状动脉狭窄程度分级
一级,正常,无冠状动脉狭窄
二级,轻度狭窄,狭窄小于30%
三级,中度狭窄,狭窄介于30%~50%间
四级,重度狭窄,狭窄介于50%~90%间
五级,次全闭塞,狭窄程度大于90%
六级,完全闭塞,管腔完全闭塞,无血流通过
TIMI冠脉血流分级
TIMI 0级:无再灌注或闭塞远端无血流。
TIMI Ⅰ级:造影剂部分通过闭塞部位,梗塞区供血冠状动脉充盈不完全。
TIMI Ⅱ级:部分再灌注或造影剂能完全充盈冠状动脉远端,但造影剂进入和清除的速度都较正常的冠状动脉慢。
TIMI III级:完全再灌注,造影剂在冠状动脉内能迅速充盈和清除。
常用造影导管
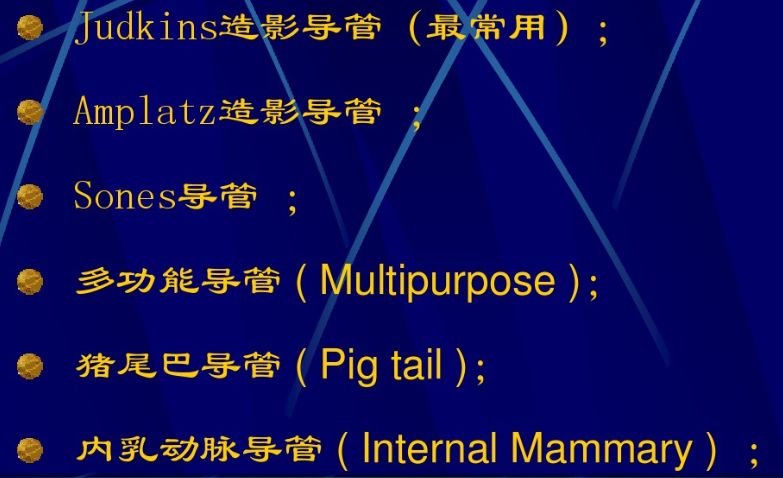
造影用的心导管主要有:猪尾巴导管、侧孔造影导管、端侧孔造影导管、漂浮球囊造影导管及状动脉造影导管,小儿常用F5和F6导管。
导管对应尺寸换算表

手术的大致过程
操作时一般经皮穿刺股动、挠动脉。将导管送到选择造影的部位。导管在血管及心腔中时要用肝素盐水(500ml中含肝素40mg)冲洗滴注于心导管内以防导管凝血,如做左心系统造影,导管置入动脉系统中即应从导管中推入0.5mg/kg的肝素进行抗凝,防止血栓形成和栓塞。造影完毕后退出心导管在要穿刺部位按压止血,至不再出血 加压包扎,以免形成血肿。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












初学者的解惑好文
50
#冠状动脉造影#
63
#造影#
56
不错
65
好文章
57
好
76
#心血管#活
64
#心血管#好
71
受益匪浅
50